Mental illness is any disease of the mind or brain that seriously affects a person’s thoughts, emotions, personality, or behavior. Symptoms of mental illness may include extreme moods, such as excessive sadness or anxiety, or a decreased ability to think clearly or remember well. Almost everyone experiences mood swings or finds it difficult to think clearly from time to time. A mentally ill person, however, has severe symptoms that damage the person’s ability to function effectively in everyday activities and situations.
Mental illness has many forms, and it affects people in all nations and at all economic levels. In the United States, approximately 3 percent of the population have a severe mental illness. But about 40 percent of Americans will experience a mental illness at some time in their lives. Although milder mental illnesses sometimes pass without treatment, severe cases of mental illness require professional treatment.
Mental health professionals have made important advances in the treatment of mental illness since 1950. Treatment methods used today usually help people recover from their symptoms more quickly than in the past. The availability of effective treatment has helped to reduce the fear, disgrace, and shame that has surrounded mental illness for centuries. Most people with mental illness can return to leading normal, productive lives after obtaining appropriate treatment.
Mental health professionals sometimes refer to mental illnesses as mental disorders or psychiatric illnesses. The terms neurosis and psychosis are sometimes used to describe the severity of various mental illnesses. A neurosis is a mild disorder that causes distress but does not interfere greatly with a person’s everyday activities. A psychosis is a severe mental disorder that prevents an individual from functioning in a normal manner. Insanity is a legal rather than a medical term, which is used to describe a mental illness so severe that the person is considered not legally responsible for his or her acts. In everyday language, people may call a mental illness that occurs suddenly and requires rapid treatment a nervous breakdown, but mental health professionals do not use this term.
Kinds of mental illnesses
There are many different kinds of mental illnesses. The standard classification systems describe more than 100 types of mental disorders, which are divided into broad categories. These categories include delirium, dementia, schizophrenia, mood disorders, anxiety disorders, dissociative disorders, somatoform disorders, personality disorders, eating disorders, and substance use disorders.
Delirium
is a disorder in which a person loses awareness of his or her surroundings. People with delirium are easily distracted and confused. At times they do not know where they are or who they are, and they act and speak in a disorganized manner. People usually develop this disorder during a serious physical illness. Causes of delirium include infection, head injury, liver or kidney disease, and drug use or drug withdrawal. Most delirium cases begin suddenly and last no longer than a week.
Dementia
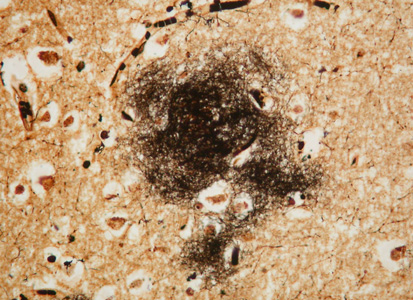
is characterized by a decrease in mental ability, especially memory and judgment. People with dementia may forget names, conversations, or recent events. They often neglect personal hygiene and disregard social rules. Dementia occurs mainly in elderly people and results from illnesses that destroy brain tissue, such as Alzheimer’s disease.
Schizophrenia
is a severe mental disorder that affects many aspects of thinking, emotion, perception, and behavior. This mental illness is defined by the presence of one or more characteristic symptoms, such as hearing voices when no one is around or irrationally feeling persecuted. These symptoms are usually accompanied by a significant decline in the ability to function in many areas, including work, school, and relationships with other people.
The characteristic symptoms of schizophrenia can be divided into (1) positive symptoms and (2) negative symptoms. Positive symptoms represent distortions or exaggerations of normal emotions or mental abilities. They include hallucinations, delusions, disorganized speech, and disorganized or peculiar behavior. Negative symptoms represent a decrease in or loss of normal emotions or mental abilities. They include decreased speech, dulled emotions, and difficulty in beginning and completing goal-directed activities.
Schizophrenia usually strikes during the late teens or early 20’s. The exact cause of schizophrenia remains unknown. Evidence suggests that physical or chemical changes in the brain are involved. These changes are difficult to reverse completely with the treatment methods currently available. Medical studies suggest schizophrenia may actually be several distinct mental disorders based on genetic (hereditary) factors. The wide range of symptoms may result from underlying genetic variation among people with the disorder.
Mood disorders,
also known as affective disorders, mainly involve disturbances in the person’s mood. The two chief mood disorders are major depression (extreme sadness) and mania (extreme happiness and overactivity). People with bipolar disorder, also called manic-depressive illness, suffer from alternating periods of depression and mania. Mood disorders are usually episodic—that is, the person experiences mood disturbances at relatively brief, distinct periods during the course of the illness. People with mood disorders typically return to normal levels of functioning after treatment.
Most people with depression feel sad, hopeless, and worthless. Many also suffer from insomnia and loss of appetite and have trouble concentrating. Some people with depression move and think slowly, but others feel restless. Some feel so hopeless and discouraged that they consider or attempt suicide. About 15 percent of people who seek treatment for depression commit suicide.
A person with mania appears excessively and inappropriately happy and confident. The happy mood may shift suddenly to irritability, sometimes leading to angry outbursts. The person’s thoughts may jump from one topic to another, producing rapid and rambling speech. People with mania move quickly, work energetically, and need little sleep. They shift restlessly from project to project but seldom complete any particular task. Most periods of mania begin suddenly, last for a few days or weeks, and then end abruptly.
Anxiety disorders
are mental illnesses in which a person experiences excessive and unreasonable fear and anxiousness. They include (1) panic disorder, (2) obsessive-compulsive disorder, (3) generalized anxiety, and (4) phobias.
Panic disorder
is characterized by panic attacks (sudden periods of intense fear). Symptoms of panic attacks include shortness of breath, rapid heartbeat, dizziness, numbness, sweating, and trembling. A fear of death often accompanies these physical disturbances. Most panic attacks last several minutes. Many people experience a panic attack at some time in their lives, but this does not mean that they have a disorder. Panic disorder results when the number of attacks or the persistent fear that another attack will occur makes it difficult for someone to carry out normal daily activities. For example, a man with panic disorder may refuse to go to work because he fears that he might have an attack while driving his car.
Obsessive-compulsive disorder
is characterized by illogical and uncontrollable thoughts or impulses that result in obsessions or compulsions. Obsessions are persistent thoughts that the person considers senseless or terrible but cannot ignore. The most common obsessions include thoughts of committing violent acts or becoming infected by germs. Compulsions are actions performed again and again with little purpose, such as repeated hand washing or counting objects.
People with compulsions sometimes believe their actions will produce or prevent some future event. For example, a girl may believe her father will die if she does not perform a series of ritualistic actions each day. People with compulsions usually realize the senselessness of their behavior and do not enjoy performing the repetitive rituals. In severe cases, the compulsion becomes the person’s major activity and thus prevents the individual from leading a normal life.
Generalized anxiety
is a persistent fear without obvious cause that lasts 6 months or longer. Its symptoms include muscle tension, nausea, rapid heartbeat, and hot or cold spells. People with generalized anxiety constantly worry that something terrible will happen to them. This makes them impatient and irritable, and they may find it difficult to get along with other people.
Phobias
are persistent, strong fears of certain objects or situations. Common phobias include agoraphobia (the fear of large open spaces) and claustrophobia (the fear of small enclosed spaces). A person suffering from a phobia has a strong desire to avoid the dreaded object or situation. If forced into contact with the cause of the phobia, the individual may panic. Most people have at least one phobia. Phobias become a disorder when they seriously interfere with a person’s daily activities.
Dissociative disorders
involve a loss or change of memory or identity. In a dissociative disorder called psychogenic amnesia, a person forgets his or her past. In a similar disorder, called psychogenic fugue << fyoog >> , the individual not only forgets the past but also travels away to live in a new location and assumes a new identity. People who suffer from depersonalization disorder feel as if they are watching themselves from a distance and have no control over their actions. In multiple personality disorder, the individual has two or more distinct personalities, each of which dominates at certain times.
Somatoform disorders
are mental illnesses in which a person experiences physical symptoms with no explainable cause. Symptoms that commonly occur in somatoform disorders include chest pain, shortness of breath, sexual problems, and muscle weakness or paralysis. People who suffer from a somatoform disorder called hypochondriasis constantly fear disease. They interpret minor symptoms as indicators of serious illnesses. Patients with somatoform disorders may persistently seek unnecessary medical treatments, including medication and surgery.
Personality disorders
are characterized by behavioral traits that create significant difficulties in personal relationships. For example, antisocial personality disorder is characterized by aggressive and harmful behavior that first occurs before the early teens. Such behavior includes lying, stealing, fighting, and resisting authority. During adulthood, people with this disorder often have difficulty keeping a job or accepting responsibility.
People with borderline personality disorder often have unstable personal relationships, problems with self-identity, and very noticeable mood changes. They may also act impulsively in potentially self-damaging ways, such as shoplifting, drug use, or reckless driving.
Individuals who suffer from paranoid personality disorder are overly suspicious, cautious, and secretive. They may believe that people are watching them or talking about them. They often criticize others but have difficulty accepting criticism.
People with obsessive-compulsive personality disorder attach great importance to being organized. They strive for perfection and efficiency and may spend much time making lists and schedules. But they are indecisive, and their concern for details keeps them from accomplishing much outside of a narrow area of focus. They often make unreasonable demands on others and have difficulty expressing emotions.
Eating disorders
include anorexia nervosa and bulimia. Both of these disorders are characterized by an extreme fear of gaining weight or becoming fat. Both are much more common in women than men and are especially common in the teen years. A girl with anorexia nervosa has a distorted image of her body, believing that she is fat even though her weight is below normal. She will do whatever she can to lose more weight, including dieting, fasting, or exercising. In severe cases, this condition is life-threatening. People with bulimia have frequent and uncontrollable periods of overeating called binges. After binging, most people with bulimia make themselves vomit or use laxatives to prevent weight gain.
Substance use disorders
involve the abuse of alcohol and certain other drugs, including amphetamines, barbiturates, cocaine, and heroin. Because drug abuse physically affects the brain, it can cause extreme changes in a person’s behavior, mood, and personality. Mental illnesses that may result from substance abuse include delirium and mood disorder.
After continued use of drugs, people may become addicted to them. This drug dependence can be psychological, physical, or both. People who use such drugs as alcohol and heroin may develop withdrawal symptoms if they stop using them. Typical withdrawal symptoms include nausea, vomiting, seizures, dizziness, and fever.
Causes of mental illness
Mental illnesses have various causes. Some mental illnesses are due to physical changes in the brain resulting from illness or injury. Chemical imbalances in the brain may cause other mental illnesses. Genetic factors and psychological and social factors also may play important roles in certain mental illnesses. Most researchers believe that the majority of mental disorders result from a combination of two or more causes.
Physical changes in the brain
may cause a number of severe mental disorders, including delirium and dementia. Brain damage can result from head injuries, infections, or inherited defects. Diseases that damage or destroy brain tissue include encephalitis, meningitis, and brain tumors.
Chemical imbalances in the brain
may also trigger mental illnesses, particularly schizophrenia, mood disorders, and some of the anxiety disorders. These imbalances occur when brain processes involving chemicals called neurotransmitters develop a malfunction. Important neurotransmitters include dopamine, serotonin, norepinepherine, gamma-amino-butyric acid, and glutamate. Neurotransmitters act as chemical messengers and enable nerve cells in the brain to communicate with one another. People with schizophrenia may have an abnormal amount of dopamine or an imbalance between dopamine and serotonin. Researchers believe that these and other neurotransmitters also play a role in mania, depression, anxiety disorders, and personality disorders.
Genetic factors.
Research has shown that schizophrenia and mood disorders sometimes run in families. This evidence indicates that children who inherit certain genes from their parents may develop these mental illnesses. These genes probably control the production of chemicals in the brain or the way nerve cells form connections with one another in the brain. The disorder may not occur, however, unless certain environmental conditions are also present. Thus, a variety of factors may determine whether a person with an inherited tendency will actually become mentally ill.
Social and psychological factors
that may increase the probability that a person will have a mental illness include early life experiences and various types of stress. Early life experiences, such as the loss of a parent, may affect an individual’s ability to adapt to changes or to recover from painful events. Some common stresses that may contribute to the development of mental illness include difficulties in school or at work, poor health, financial problems, or family responsibilities.
Treatment of mental illness
Most people with mental illness require specialized treatment from mental health professionals, such as psychiatrists, psychologists, psychiatric social workers, or psychiatric nurses. Psychiatrists have an M.D. degree and advanced training in the treatment of mental illness. Psychologists have a doctor’s or master’s degree and may have practical clinical training that qualifies them to perform treatment. Most other mental health professionals have a bachelor’s or master’s degree and specialized training in counseling or rehabilitation.
Mental health professionals use a number of treatments for mental illness. The two main types of treatments are (1) somatic therapy and (2) psychotherapy. Most patients do not require inpatient hospital care and can be treated within their home community as outpatients. Treatment for extremely severe mental disorders, however, may require hospitalization.
Somatic therapy
usually involves the use of medications. These medications provide the foundation for the treatment of severe mental illnesses. Most of them work by changing the balances of the brain’s neurotransmitters. Another form of somatic therapy is electroconvulsive therapy, which involves passing an electric current through the brain. Both treatment with medications and electroconvulsive therapy must be administered by mental health professionals with medical training, usually psychiatrists.
Medication treatment.
Since 1950, scientists have developed a number of medications that have proved extremely successful in the treatment of certain mental disorders. Psychiatrists use heterocyclic antidepressants and selective serotonin reuptake inhibitors (SSRI’s) to treat patients with severe depression. In most cases, these medications restore the depressed patient to a normal level of functioning.
Lithium carbonate is the most effective drug for patients who suffer from bipolar disorder. It reduces the frequency and severity of both the manic and depressive periods and, in some cases, eliminates them entirely.
Medications called antianxiety drugs help relieve the tension caused by anxiety disorders. Increasingly, SSRI’s are also used in the treatment of anxiety disorders and some personality disorders.
Psychiatrists use antipsychotic drugs to treat schizophrenia. These medications help relieve certain positive symptoms of schizophrenia, such as hallucinations and delusions. However, most antipsychotic drugs prove less effective in the treatment of negative symptoms.
The medications used to treat mental disorders may have side effects. Drowsiness may accompany the use of antianxiety drugs, and antipsychotic drugs may cause restlessness and muscle spasms. Some antidepressants may produce drowsiness and weight gain. Medication treatment may be discontinued after the symptoms of the disorder have diminished or stopped. In some cases, however, the symptoms then return, and the patient must resume taking medication.
Electroconvulsive therapy (ECT)
is used primarily for the treatment of severe depression. Psychiatrists usually use it to treat hospitalized patients who remain depressed and suicidal in spite of medication treatment and psychotherapy. In most cases, ECT shortens the period of depression, but the patient must often take medication for some period of time after ECT treatment to reduce the risk of relapse.
An ECT treatment consists of passing an electric current through the patient’s brain for a fraction of a second. Prior to treatment, the patient is given anesthesia and a drug that prevents convulsions. Typically, a patient receives such treatments two to three times a week, with a total of 6 to 10 treatments. After treatment, the patient experiences temporary amnesia and confusion. Mild problems with memory may persist for several months. ECT has aroused controversy due to concern about its side effects, but most psychiatrists believe it is an effective form of treatment for severe depression.
Psychotherapy
is a form of treatment that uses psychological methods. For example, a patient in psychotherapy might try to achieve insight into unconscious thoughts or to learn more adaptive ways of responding or behaving. Psychotherapy may be used alone or in conjunction with medication treatment. The chief kinds of psychotherapy include (1) psychodynamic, (2) behavioral, (3) cognitive, (4) supportive, (5) group, (6) rehabilitative, and (7) play.
Psychodynamic psychotherapy
is based on the theory that symptoms of mental illness result from conflicts between conscious and unconscious forces in the mind. The best-known form of psychodynamic therapy is called psychoanalysis. Psychoanalysts try to make their patients aware of unconscious mental conflicts and help them find ways to resolve these conflicts. Many analysts use a method called free association, in which the patient talks about anything that comes to mind. A psychoanalyst may also explore dreams and childhood memories, which can provide insight into unconscious thoughts and feelings.
Behavioral therapy
concentrates on relieving current symptoms of the patient’s mental illness without trying to understand unconscious conflicts. Behavioral therapists help patients develop appropriate behavior through such methods as rewarding desirable responses and ignoring undesirable ones.
Cognitive therapy
focuses on teaching patients how to retrain their thinking patterns. Cognitive therapists help patients to eliminate negative and undesirable thoughts and to improve self-esteem.
Supportive psychotherapy
focuses on recent events and personal relationships in the patient’s life. The patient and the therapist work as a team to solve problems. Supportive therapists provide reassurance and try to help patients appreciate and accept themselves.
Group therapy
is conducted with a group of people, usually from 4 to 12. A therapist leads and guides the group. Many patients learn about their own problems by sharing experiences with people who have similar conflicts. The group members also encourage and support one another during times of personal stress.
Rehabilitative therapy
focuses on teaching patients new skills and abilities. Patients with severe mental illnesses may need help in learning to deal with practical aspects of daily living, such as finding work, obtaining adequate housing, or managing finances. Social workers and rehabilitation counselors generally provide this type of therapy. It usually is offered in a community setting, such as a community mental health center.

Play therapy
is used in treating mentally disturbed children. A therapist gives the child dolls and other toys and asks the youngster to tell a story about them. The child generally uses the toys to act out personal conflicts. The therapist then helps the young patient relate these play actions to his or her own situation.
Treatment settings.
Mental health professionals usually provide treatment within the patient’s home community. Hospitalization may be required, however, for those who need intensive medical attention or who might harm themselves or others. For example, patients whose symptoms include suicidal or violent behavior may require hospitalization.
In a hospital setting, the medical staff can carefully monitor medication treatment. Furthermore, patients can begin rehabilitative programs that help them deal with the psychological and social consequences of their illnesses. In the past, patients with severe mental illnesses were hospitalized for long periods of time. Today, however, medications and ECT provide effective treatments for many of these disorders. As a result, most patients remain in the hospital for only a few days or weeks.
Community treatment programs developed as a complement to hospitalization treatment for the severely mentally ill. Types of community-based programs include vocational rehabilitation, day hospital programs, and group homes in which patients reside together. Rehabilitation counselors, social workers, psychologists, or psychiatrists usually provide community treatment.
Many areas do not have an adequate number of community treatment programs. This has contributed to an increase in the number of homeless mentally ill people. Mental health professionals working at community centers try to help the homeless mentally ill find food and shelter and readapt to life in a community.
History
Early attitudes.
Prehistoric peoples apparently believed mental illnesses were caused by evil spirits that possessed the body. They may also have believed that drilling a hole into the person’s skull would release the evil spirits. Scientists have found fossils of drilled skulls that date back as far as 10,000 years.
About 400 B.C., the Greek physician Hippocrates stated that mental disorders resulted from an imbalance of four body fluids: blood, phlegm, yellow bile, and black bile. For example, depression supposedly resulted from an excess of black bile. The ancient Greek name for this fluid, melan chole, is the origin of the word melancholy, which means sadness.
During the Middle Ages, a belief in witchcraft spread throughout Europe. Many people with mental illness were considered to be witches and were killed by burning, hanging, or drowning. Mentally ill people were also put in prisons or in government welfare institutions called poorhouses.
During the 1500’s, many European nations built special institutions to separate the mentally ill from the rest of society. One of the most famous of these institutions was St. Mary of Bethlehem in London, which was widely known as Bedlam. The inmates there suffered from unsanitary conditions, beatings, and other harsh treatment. Today, the word bedlam means uproar and confusion.
Humane treatment
of mentally ill people gained importance in the late 1700’s. During that period, Philippe Pinel, a French physician, and William Tuke, a British merchant, worked to improve the conditions of mental institutions in their countries. Through their efforts, many mental hospitals introduced treatment programs that included fresh air and pleasant surroundings.

During the early 1800’s, American physician Benjamin Rush incorporated the ideas of Pinel and Tuke in treating mentally ill patients at Pennsylvania Hospital in Philadelphia. Dorothea Dix, an American schoolteacher, began visiting mental hospitals throughout North America and Europe in the mid-1800’s. She described the miserable conditions in these hospitals to state legislators and persuaded them to pass laws providing state funds for mental institutions.
Medical approaches
to mental illness were first practiced in ancient Greece and Rome and again became standard practice in the late 1800’s in Europe. Emil Kraepelin, a German psychiatrist, presented a system of diagnosing and classifying mental disorders in 1883. He also advanced the search for the causes of mental illness through his study of mental disorders and changes in the brain.
In the early 1900’s, Austrian psychiatrist Sigmund Freud introduced the theory that forces in the unconscious mind strongly influence an individual’s personality and behavior. Freud also suggested that conflicts during early childhood affect the development of the unconscious. These theories became the basis for psychoanalysis and other forms of psychotherapy.
Recent developments.
During the 1950’s, the discovery of effective medication treatments led to a reduction in the number of patients in hospitals and state institutions built for the care of the mentally ill. In 1956, for the first time, the number of patients discharged from public mental hospitals in the United States exceeded the number admitted. Many communities, however, lacked adequate services and facilities to help mentally ill people readjust to living independently.
The Community Mental Health Centers Construction Act of 1963 provided funding for the development of community mental health centers throughout the United States. Although this act led to improved community services, it failed to ensure that the nation’s health care system would provide treatment for mental illnesses equal to that provided for physical illnesses. As a result, many people with mental illnesses still cannot obtain or afford adequate treatment.
Mental health professionals, patients, and family members have formed organizations committed to improving public understanding of mental illness. The National Alliance on Mental Illness, one of the earliest of these groups, was established in 1979. During the 1980’s and 1990’s, many scientists began to study the living brain with new techniques, including positron emission tomography (PET) and magnetic resonance imaging (MRI). Images created with these technologies have shown that many mental illnesses involve problems in brain development, structure, or function.
