Antibiotic << `an` tee by OT ihk or `an` tih by OT ihk >> is a substance produced by certain bacteria or fungi that kills other cells or interferes with their growth. In nature, these substances help some microbes survive by limiting the multiplication of other microbes that share the same environment. Antibiotics that attack pathogenic (disease-causing) microbes without severely harming normal body cells are useful as drugs.
Antibiotics are especially useful for treating infections caused by bacteria. Antibiotics came into widespread use during the 1940’s. At that time, they were often called “wonder drugs” because they cured many bacterial diseases that were once fatal. The number of deaths caused by meningitis, pneumonia, tuberculosis, and scarlet fever declined drastically after antibiotics became available. Today, physicians prescribe antibiotics to treat many diseases caused by bacteria.
In addition, some antibiotics are effective against infections caused by fungi and protozoa, and a few are useful in treating cancer. Antibiotics are also used to treat infectious diseases in animals. Farmers sometimes add small amounts of antibiotics to livestock feed. The antibiotics support the animals’ growth for reasons that are not entirely understood.
Antibiotics are not effective against colds, influenza, or other viral diseases. In addition, the effectiveness of antibiotics is limited because both pathogenic microbes and cancer cells can become resistant to them.
Kinds of antibiotics
Antibiotics are selectively toxic—that is, they damage some types of cells without harming others. Medically useful antibiotics attack infectious microbes or cancer cells without excessively hurting human cells. Antibiotics fight different types of illnesses in a variety of ways.
Antibacterial antibiotics.
Antibiotics are selectively toxic against bacteria because bacterial cells differ greatly from human cells. One of the chief differences is that bacteria, unlike animal cells, have a cell wall. This wall is a rigid structure that forms the cell’s outer boundary.
The type of cell wall a bacterium has is one factor that determines which antibiotics can kill it. Scientists use a process called Gram staining to classify cell walls of bacteria. Hans C. J. Gram, a Danish bacteriologist of the late 1800’s, developed the process. This method classifies bacteria as gram-positive (G+) or gram-negative (G-).
Some antibiotics selectively kill either gram-positive bacteria or gram-negative bacteria. These substances are called narrow spectrum antibiotics. The antibiotic Vancomycin << `van` koh MY sihn >> selectively kills such gram-positive bacteria as Staphylococcus << `staf` uh luh KOK uhs >>, Streptococcus << `strehp` tuh KOK uhs >>, and Enterococcus << `ehn` tuhr oh KOK uhs >>. Aztreonam << az TREE oh nahm >> is a narrow spectrum antibiotic that kills only gram-negative bacteria, such as Escherichia coli << `ehsh` uh RIHK ee uh KOH ly >> and Pseudomonas aeruginosa << `soo` duh MOH nas ih ROO juh `noh` suh >>. Other antibiotics can kill both gram-positive and gram-negative bacteria. These drugs are called broad spectrum antibiotics. Ceftriaxone << sehf try AHKS ohn >> is one example of a broad spectrum antibiotic. No broad spectrum antibiotic can kill all bacteria, and no narrow spectrum antibiotic can kill all gram-positive or all gram-negative bacteria.
Other kinds of antibiotics.
Some antibiotics are effective against infections caused by fungi and protozoans, whose cells differ from human cells. Antibiotics that fight fungi include miconazole << mih KON ah zohl >> and amphotericin << `am` fuh TEHR uh sihn >>. Paromomycin << `par` oh moh MY sihn >> is used to treat amebiasis << `am` uh BY uh sihs >>, an intestinal disease caused by a protozoan.
Anticancer antibiotics attack cells while they are dividing. These drugs are somewhat selectively toxic because cancer cells generally divide much more frequently than do normal cells. But some normal cells—such as blood-forming cells—divide rapidly. Anticancer antibiotics also affect these cells. The antibiotic doxorubicin << DOK soh `roo` buh sihn >> is used to treat certain types of leukemia, breast cancer, and other tumors.
How antibiotics work
Antibiotics fight microbes and cancer cells by interfering with normal cell functions. In most cases, this interference occurs in one of three ways: (1) prevention of cell wall formation, (2) disruption of the cell membrane (covering), and (3) disruption of chemical processes.
Prevention of cell wall formation.
Penicillins and some other antibiotics destroy microbes by interfering with their cell wall formation. Animal cells do not form walls. As a result, these antibiotics do not damage them.
Disruption of the cell membrane.
All cells have a membrane that controls the movement of substances in and out of the cell. Some antibiotics, including amphotericin B and nystatin, disrupt the cell membrane of certain microbes. A damaged membrane might allow vital nutrients to escape or poisonous substances to enter and kill the cell. These antibiotics do not harm human cells because the drugs affect membrane components found only in microbial cells.
Disruption of chemical processes.
All cells produce proteins and nucleic acids, which are vital to life. Human cells produce these substances in much the same way as microbial cells do. But in some cases, these processes differ enough so that antibiotics interfere with the chemical activities in microbial cells, but not in human cells. For example, streptomycin << `strehp` tuh MY sihn >> and tetracycline << `teht` ruh SY kleen or TEHT ruh `sy` klihn >> prevent certain kinds of microbes from producing proteins, and rifampin << RIHF am pihn >> interferes with the formation of nucleic acids.
Dangers of antibiotics
Many antibiotics are regarded among the safest drugs when properly used. But antibiotics can sometimes cause unpleasant or dangerous side effects. The three main dangers are (1) allergic reactions, (2) destruction of helpful microbes, and (3) damage to organs and tissues.
Allergic reactions,
in most cases, are mild and produce only a rash or fever. But severe reactions can occur, and can even cause death. All antibiotics are able to produce allergic reactions, but such reactions occur most often with penicillins. A physician usually asks if a patient has ever had an allergic reaction to an antibiotic before prescribing that drug. Most people who are allergic to one antibiotic can take other antibiotics that have significantly different chemical compositions.
Destruction of helpful microbes.
Certain areas of the body commonly harbor both harmless and pathogenic microbes. These two types of microbes compete for food, and so the harmless microorganisms help restrain the growth of those that cause disease. Many antibiotics—especially broad spectrum drugs—do not always distinguish between harmless and dangerous microbes. If a drug destroys too many harmless microorganisms, the pathogenic ones will have a greater chance to multiply. This situation can lead to a new infection called a superinfection. Physicians usually prescribe a second drug to combat a superinfection.
Damage to organs and tissues
is rare in people using antibiotics that act only against the cells of pathogenic microbes. Extensive use of some antibiotics, however, may damage tissues and organs. For example, streptomycin has caused kidney damage and deafness. Physicians prescribe drugs with such known risks only if no other drug is effective.
Anticancer antibiotics act against all cells that divide rapidly, and so can affect normal cells as well as cancer cells. For example, cells in the bone marrow divide constantly to produce fresh blood cells. Anticancer antibiotics can damage the bone marrow. Such damage increases the risk of infection by reducing the number of white blood cells, which help the body fight disease.
Resistance to antibiotics.
Some pathogenic microbes develop an ability to resist the effects of certain antibiotics. The most widespread and worrisome resistance in pathogenic microbes occurs in bacteria.
Bacteria can become resistant to antibiotics through a type of evolution. In bacteria—as in other living things—genes carry instructions controlling life processes. Occasionally, a gene in a bacterium naturally changes in a way that enables the microbe to resist the effects of an antibiotic. Such a change is called a mutation. The change may provide resistance to one specific antibiotic or to a group of chemically similar antibiotics—for example, the penicillins. Bacteria can also acquire resistance from other bacteria by transferring genetic material. In some cases, these exchanges enable bacteria to acquire resistance to more than one type or more than one group of antibiotics.
Bacteria also can become resistant to antibiotics by producing an enzyme that breaks down the drug. This occurs with Staphylococcus, which may resist penicillins and cephalosporins << `sehf` uh luh SPAWR ihnz >>. Bacteria can also change their cell membranes so that antibiotics can not penetrate them. An example of this kind of bacteria is Pseudomonas. Pseudomonas may develop resistance to the quinolone antibiotics this way. Enterococcus, a gram-positive bacteria, can become resistant to vancomycin by changing the proteins to which vancomycin usually binds. Streptococcus can resist penicillins and cephalosporins in this way.
Testing and producing antibiotics
Testing.
Every year, scientists test thousands of natural and chemically modified microbial substances for potential use as antibiotics. First, they test these substances against harmful microbes or cancer cells that have been grown either in test tubes or on laboratory plates.
A substance that shows strong antibiotic activity against pathogenic microbes or cancer cells undergoes extensive tests in laboratory animals. If it produces no harmful effects in the animals, scientists test the antibiotic in human beings. In the United States, the Food and Drug Administration (FDA) must approve human testing. If the drug proves to be safe and effective, it is referred to the FDA for approval. Finally, if the FDA approves the antibiotic, the developer begins to produce it for sale.
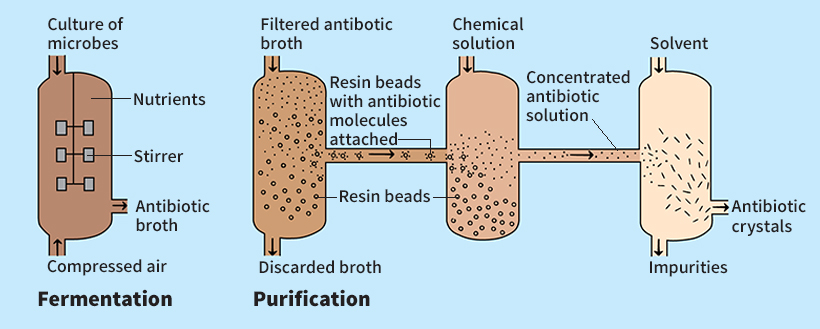
Production
of antibiotics involves several steps. First, cultures of antibiotic-producing microbes are grown in flasks and then transferred to huge fermentation vats (see Fermentation). The microbes multiply rapidly in the vats because the environment is controlled to stimulate their growth. After fermentation, the antibiotic substance is extracted from the culture and purified.
Some natural antibiotic substances are modified chemically to produce semisynthetic antibiotics. Many such drugs are more effective than the natural antibiotics from which they were developed.
Drug companies conduct special tests on antibiotics during and after production to ensure their quality. Finally, manufacturers make the purified antibiotic substances into pills, liquids, and ointments for medical use.
History
For more than 2,500 years, people have treated certain skin infections with molds that form antibiotics. However, modern scientific study of these substances did not begin until the late 1800’s. At that time, the French chemist Louis Pasteur discovered that bacteria spread infectious diseases. Then Robert Koch, a German bacteriologist, developed methods of isolating and growing various kinds of bacteria. Koch also identified specific bacteria that cause certain diseases.
Scientists then began working to develop drugs that could destroy pathogenic microbes, but the substances they produced proved either ineffective or dangerous. A historic breakthrough came in 1928, when British bacteriologist Alexander Fleming observed that a mold of the genus Penicillium produced a substance that destroyed bacteria. He called the substance penicillin.

In the early 1940’s, American bacteriologist Selman A. Waksman tested about 10,000 types of soil bacteria for antibiotic activity. In 1943, he discovered that some Streptomyces << strehp tuh MY seez >>, a type of fungi, produced a substance that had potent antibiotic properties. A new antibiotic called streptomycin resulted from Waksman’s research. Thousands of antibiotic substances have been found in nature or have been produced chemically. Relatively few antibiotic substances, however, have proved safe and effective.
Since the 1990’s, resistance to antibiotics has been a growing threat to public health. Widespread use of antibiotics to treat human infections increases the number of resistant bacteria. Antibiotic use in livestock promotes the development of resistant bacteria that can spread to humans. For example, studies in the Netherlands, Spain, the United States, and the United Kingdom in the late 1990’s revealed that many chickens were infected with antibiotic resistant strains of a bacterium called Campylobacter << `KAM` pih loh BAK tuhr >>. When people cooked the meat of these chickens, some of the Campylobacter microbes survived, and the people became infected.
Certain kinds of Enterococcus bacteria are especially troublesome because of their resistance. In Europe, drug-resistant strains (types) of Enterococcus that originated in livestock have spread to people. In the United States, Enterococcus resistant to multiple antibiotics has caused human infections that are difficult or impossible to treat. Infections caused by antibiotic-resistant varieties of Enterococcus occur mostly in patients who are already seriously ill.
In the 1990’s, scientists combined the antibiotics quinupristin and dalfopristin to create a drug that works against resistant strains of Enterococcus. In 2000, the FDA approved linezolid << lyn AY zoh lid >>, the first entirely new type of antibiotic developed in more than 30 years. The antibiotic, sold under the brand name Zyvox, is effective against gram-positive bacteria, including Enterococcus, that have become resistant to all other antibiotics. In 2005, the FDA approved a new antibiotic marketed under the name Tygacil. The drug is a new class of antibiotics that work by defeating mechanisms that some bacteria use to resist existing drugs. But experts believe antibiotic-resistant Enterococcus remains a major threat to public health.
