Heart is the hard-working muscular pump whose steady action sustains life. With each beat, the heart sends blood throughout the body to carry oxygen and food to all the body’s cells. The rhythmic beating of the heart begins about seven months before birth. When the heart stops beating, we die unless some artificial method circulates and adds oxygen to our blood.
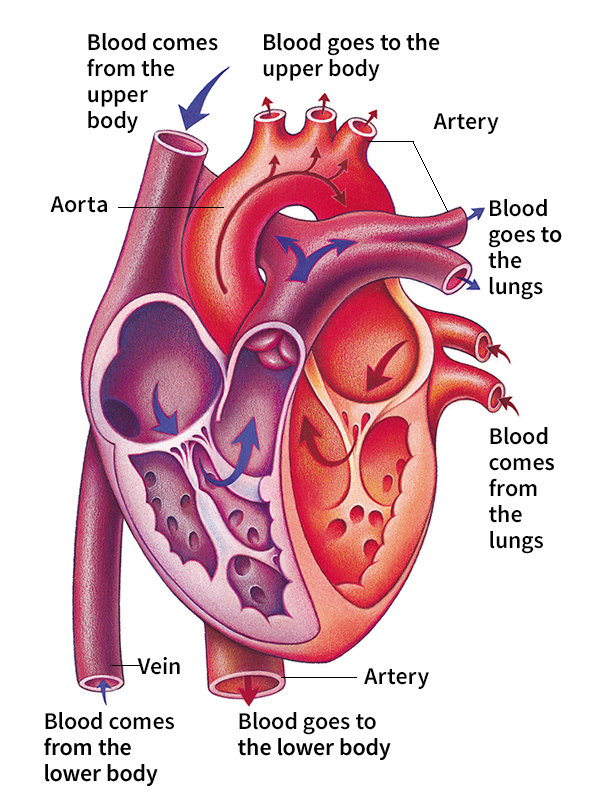
The heart is a large, hollow, muscular organ divided into left and right sides that pump at the same time. Veins collect blood from throughout the body and carry it to the right-side pump. That pump then sends blood to the lungs, where it picks up oxygen. The oxygenated (oxygen-rich) blood then flows to the left side of the heart, which pumps it through arteries to the rest of the body. Valves control the flow of blood through the heart. The left-side pump, which sends blood throughout the body, is larger and stronger than the right pump.
Loading the player...Heart beat
A division of the nervous system called the autonomic nervous system regulates the heart and blood vessels. The autonomic system controls body activities that are performed automatically, without conscious control. For example, the heart’s rate automatically increases or decreases, depending on the body’s needs. The heart pumps slowly while a person sleeps, providing relatively small amounts of oxygen to the resting body. But the heart rate can quickly speed up and greatly increase oxygen supplies when a person exercises, becomes frightened, or needs to fight or run.
Disease can strike any part of the heart. Although the death rate has fallen, disorders of the heart and blood vessels remain the leading cause of death in the United States and many other countries. The most common heart disease narrows the arteries that supply the heart itself with blood and oxygen. Deposits of fatty material gradually build up and block these arteries. If the heart receives too little oxygen, it may work poorly or even die. Damage to the heart muscle resulting from lack of oxygen is called a heart attack. A mild heart attack may force a person to lead a less active life, and a severe attack may cause death.
Medicine has made some of its most exciting advances in cardiology, the medical field that deals with diseases of the heart and blood vessels. For much of human history, doctors knew little about how the heart worked or how disease could affect the organ. In the 1900’s, doctors learned to diagnose and treat many heart conditions that once meant death. Discoveries of new drugs and great progress in surgery have added years to the lives of many heart patients. Doctors have transplanted hearts and even developed machines that can temporarily do the work of the heart.
Doctors have also learned that people can take important steps to protect the health of their hearts. Most people can greatly reduce their risk of heart disease by exercising regularly, avoiding smoking, and limiting the amount of fat and calories in their diets.
Today, much research in cardiology focuses on learning more about the causes of heart disease so that much illness can be prevented. Other research seeks to reduce death and disability from heart disease through further development of new medicines and surgical techniques. For patients who have untreatable disorders, research continues into improving heart transplantation and producing an effective artificial heart.
This article chiefly discusses the human heart. The last section briefly describes the hearts of insects, fish, birds, and other animals. For more information on what blood does in the body, see Blood and Circulatory system.
The structure of the heart
The heart lies between the lungs in approximately the middle of the chest. Each person’s heart is a little larger than the size of that person’s fist. A newborn baby’s heart weighs about 2/3 ounce (19 grams). An adult’s heart weighs from 9 to 11 ounces (255 to 312 grams).
Outer lining and muscle.
A membrane called the epicardium covers the outer surface of the heart. Another membrane, the pericardium, surrounds the epicardium. The pericardium completely encloses the heart and extends above the blood vessels that emerge from the top of the organ. A slippery fluid between the epicardium and the pericardium lubricates the heart and enables it to contract smoothly. Tough, fibrous bands called ligaments attach the pericardium to the spine and other internal structures to hold the heart firmly in place.
The heart consists chiefly of a special type of muscle known by the terms heart muscle, cardiac muscle, and myocardium. Heart muscle forms the strong outer walls of the organ as well as the septum, the wall that divides its left and right sides.
Heart muscle differs from the other two kinds of muscles in the body—that is, skeletal muscles and smooth muscles. Skeletal muscles, such as those in the arms and legs, are under our conscious control. They have long fibers with alternate dark and light bands called striations. Smooth muscles form the walls of the blood vessels, stomach, intestines, and most other internal organs. These muscles lack striations, and we do not consciously control them—they work automatically. Heart muscle, like skeletal muscle, has striations, but it contracts and relaxes automatically like smooth muscle. In addition, heart muscle cells work together so that a wave of contraction travels smoothly through the entire heart. These coordinated contractions keep the heart beating continuously and rhythmically throughout a person’s life.
Chambers, valves, and inner lining.
The muscular septum divides the heart into a left side and a right side. Movable flaps of tissue called valves further divide each side into two chambers that lie one above the other. A thin membrane called the endocardium lines the chambers. The top chambers, called the right atrium and left atrium, fill as blood returns to the heart. As each wave of contraction moves through the heart, the atria (plural of atrium) contract and squeeze blood into the lower chambers. These lower chambers are called the right ventricle and left ventricle. The contraction then forces blood out of the ventricles through the arteries. The ventricles, which must squeeze blood out of the heart, are thicker, larger, and stronger than the atria.
During each contraction, the flaps of the valves direct the flow of blood through the heart. These flaps open to let blood flow in the proper direction, then snap shut to prevent blood from flowing backwards. Two valves separate the atria and the ventricles. They are called the atrioventricular (AV) valves. The AV valve between the right atrium and right ventricle has three flaps and is called the tricuspid valve. The AV valve on the left side of the heart has two flaps and is called the mitral valve.
The heart also has valves called semilunar valves between each ventricle and the major blood vessel that carries blood away from it. Each semilunar valve has three flaps shaped like half moons. When the right ventricle contracts, it delivers blood to the pulmonary artery. The semilunar valve that controls blood flow to the pulmonary artery is known as the pulmonic valve. Because the left ventricle squeezes blood into the aorta, the semilunar valve on that side is called the aortic valve.
Blood vessels.
Blood enters and leaves the heart through several major vessels. Blood from the body flows into the right atrium through the body’s two largest veins. One, called the superior vena cava, brings blood from the head and arms. The other—the inferior vena cava—carries blood from the main part of the body and the legs. Other blood vessels transport blood between the lungs and the heart. Pulmonary veins return blood from the lungs to the left atrium. The pulmonary artery carries blood from the right ventricle to the lungs.
The aorta is the body’s largest artery. It receives oxygenated blood from the left ventricle and, through numerous branches, distributes it throughout the body. The pulmonary artery and the aorta are sometimes called the great vessels.
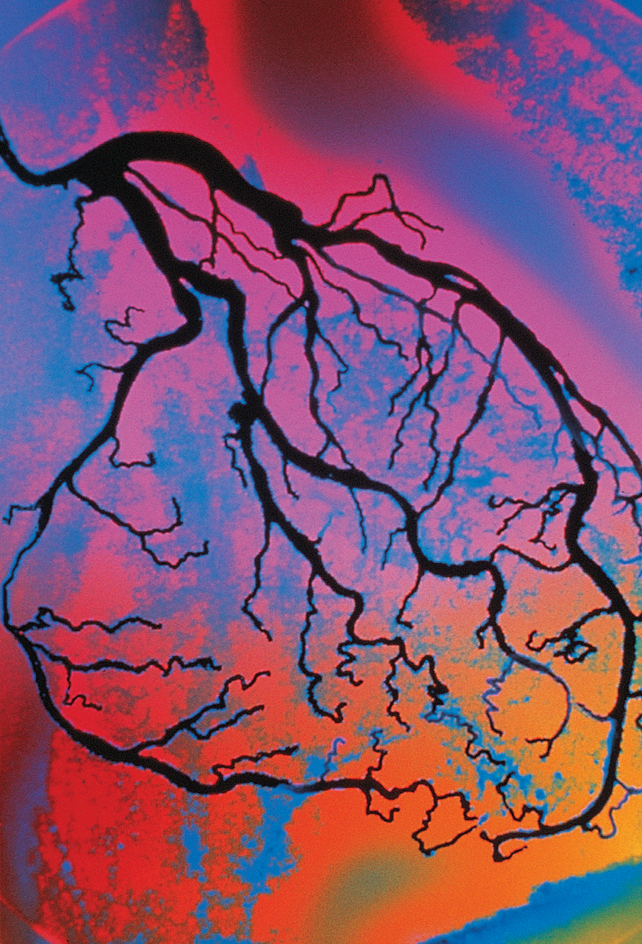
The first arteries that branch from the aorta are the two major coronary arteries. These two coronary arteries divide into many branches that cover the heart. Because these arteries nourish the heart muscle itself, diseases that affect them are among the most serious problems that cardiologists treat.
The work of the heart
Circulating blood.
The steady pumping of the heart supports life by moving blood through the body. As it flows, blood delivers food and oxygen to all the body’s cells and carries away wastes. Blood returns to the heart carrying a waste gas called carbon dioxide that cells produce as they use oxygen to obtain energy from food. Blood carrying carbon dioxide enters the right atrium through the superior vena cava and inferior vena cava. That atrium then contracts, squeezing the blood through the tricuspid valve into the right ventricle. After that ventricle fills, pressure forces the tricuspid valve to close and the pulmonic valve, leading to the pulmonary artery, to open. That ventricle then contracts, and the blood gushes through the pulmonary artery into the lungs. In the lungs, the blood releases carbon dioxide and picks up oxygen. See Lung.
Oxygenated blood from the lungs travels to the left atrium. That atrium then contracts, which squeezes the blood through the mitral valve into the left ventricle. After blood fills that ventricle, the mitral valve closes and the aortic valve opens. Blood pours into the aorta and flows through arteries to bring oxygen to the body.
Regulating the heart rate.
Both sides of the heart pump blood at the same time. As the right ventricle contracts and sends blood to the lungs, the left ventricle also contracts and squeezes blood out to the body. The heart’s cycle of activity has two stages, systole and diastole. Systole << SIHS tuh lee >> occurs when the ventricles contract. Diastole << dy AS tuh lee >> is the stage when the ventricles relax and the atria contract. One complete cycle of contraction and relaxation—called a cardiac cycle—makes up one heartbeat.
During each cardiac cycle, the heart valves open and close. Closing of the valves produces most of the “lub dub” sound of a heartbeat, which doctors can hear with an instrument called a stethoscope. As the ventricles contract, the mitral and tricuspid valves close, causing the first sound. Immediately after the valves close, pressure in the ventricles forces the aortic and pulmonic valves to open. After a contraction ends, pressure in the ventricles drops. The aortic and pulmonic valves then close, causing most of the second heart sound.
The autonomic nervous system controls the heart rate by relaying messages to the heart’s electrical signaling system. The heart’s electrical impulses (nerve signals) begin in a small bundle of specialized cells called the sinoatrial node (S-A node). The S-A node lies in the right atrium near where the superior vena cava enters the heart. The S-A node is also called the pacemaker because its rhythmic signals set the heart’s rate. Impulses from the S-A node travel along certain pathways, and the atria contract when these signals reach them. The impulse then arrives at another node, called the atrioventricular node (A-V node). The A-V node lies in the septum between the atria and ventricles. It delays the signal briefly, allowing the ventricles enough time to fill with blood. As the impulse continues, the ventricles contract.
The nerves of the autonomic nervous system control the S-A and A-V nodes. When the body needs more blood, as during vigorous exercise, the nervous system stimulates the S-A node, which increases the rate of its impulses. These impulses keep the heart chambers contracting at a faster speed, thus pumping more blood.
Resting heart rate depends on a person’s age, size, physical condition, and several other factors. A newborn baby’s heart beats about 120 times per minute. For adults, doctors consider resting rates from 60 to 100 beats per minute normal. Athletic training enlarges the heart and slows the heartbeat. Many serious athletes have resting rates as low as 40 to 60 beats per minute.
Regulating blood pressure.
Blood pressure is the force with which the blood pushes against the walls of the arteries as it circulates through the body. Each person’s blood pressure reflects the amount of blood in the body and the strength and rate of the heart’s contractions. Another important factor is the ability of the arteries to stretch in response to the force of blood.
Loading the player...Blood pressure
Blood pressure is expressed as two numbers placed one above the other. The top number, which is called systolic blood pressure, represents pressure during systole. This number is larger because it reflects the greater force created in the arteries during contraction of the ventricles. The bottom number represents lower pressure while the ventricles relax during diastole. This number is called diastolic blood pressure. To learn how blood pressure is measured, see Blood pressure.
The heart helps regulate blood pressure by producing a hormone that helps the kidneys eliminate salt from the body. Excess salt may contribute to hypertension (high blood pressure). Over many years, hypertension can damage arteries and lead to heart disease, and can also injure the brain and kidneys. See Hypertension.
Coronary artery disease
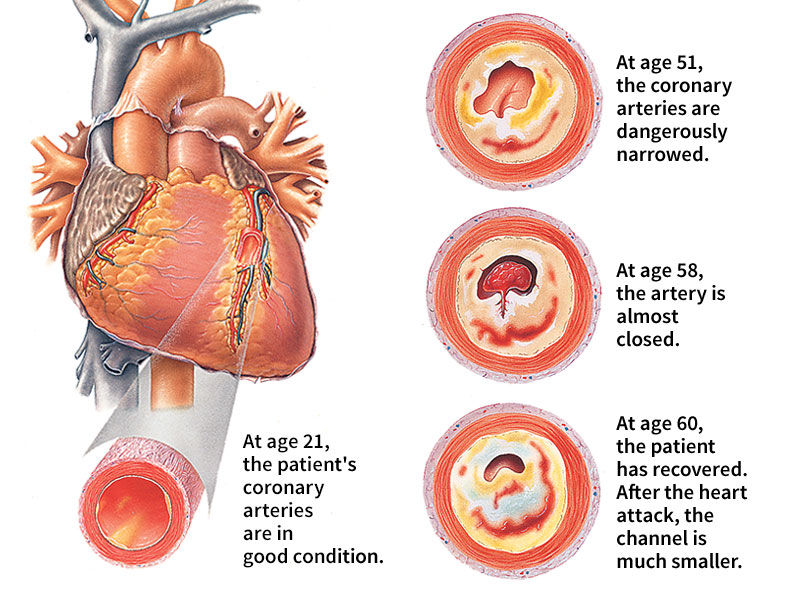
The most common heart disorder is coronary artery disease (CAD). The heart needs a constant oxygen supply because it is one of the body’s hardest-working muscles. This oxygen is delivered by the coronary arteries, which carry about 5 percent of the blood pumped from the heart directly to the heart muscle. In CAD, these arteries become narrowed, which reduces—or may even stop—their ability to carry oxygen. Insufficient oxygen may reduce the heart’s ability to pump and cause pain or damage to the heart muscle.
Causes.
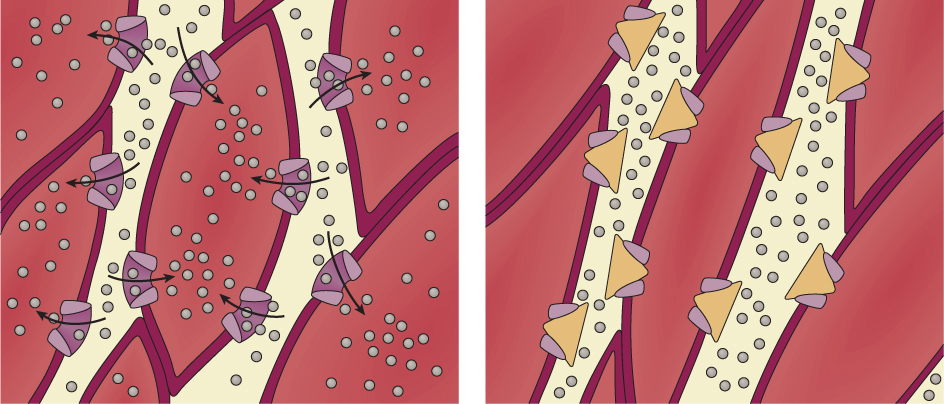
Nearly all coronary artery disease results from atherosclerosis << `ath` ur oh skluh ROH sihs >>. Atherosclerosis is a process in which deposits of fat, calcium, and dead cells form on the inner layers of artery walls. These deposits are called plaques.
Plaques interfere with the smooth flow of blood through arteries. Plaques that grow large enough can narrow an artery and significantly reduce blood flow. In some cases, plaques can block an entire artery and stop blood flow completely. Flow may also stop if a blood clot, called a thrombus, forms in the narrowed artery. Plaques often crack or break, releasing substances that also can lead to blood clots. If a blood clot blocks a coronary artery, it causes a heart attack. A clot that forms in an artery in the brain causes a stroke. See Stroke.
Risk factors.
Medical research shows that certain conditions and habits increase the likelihood that a person will develop CAD. Doctors call these conditions and habits risk factors. There are some risk factors that people cannot control. For example, CAD strikes more men than women and older people more than younger ones. In addition, doctors think that genes are involved in some cases because the disease appears to run in some families.
People can take steps to control other risk factors involved in coronary artery disease. For example, the most important risk factor is the amount of a fatty substance called cholesterol that people have in their blood. Cholesterol is one of the main fats involved in forming plaques. Doctors have found that the risk of CAD rises as a person’s cholesterol level increases. People can help control their cholesterol level by reducing the amount of cholesterol and other animal fats in their diet. For a discussion of healthy cholesterol levels, See Cholesterol.
Other controllable risk factors that may cause coronary artery disease include high blood pressure and cigarette smoking. High blood pressure stresses the heart by making it work harder, which may bring on a heart attack. In addition, the force of high blood pressure can break arterial plaques, which can also lead to blood clots and heart attacks. People can lower their blood pressure by losing weight, exercising, reducing alcohol intake, and eating less salt. Certain medicines also help reduce high blood pressure.
Cigarette smokers are more likely to develop CAD than are nonsmokers. Heavy smokers have more than twice the risk of a heart attack that nonsmokers have. But smokers who quit significantly reduce their risk of heart disease. Other risk factors that may contribute to development of coronary artery disease include diabetes, obesity (excess body fat), lack of exercise, and stress.
Regular medical checkups are an important tool in controlling risk of CAD. During examinations, doctors can check a patient’s blood pressure and cholesterol level. They can also check the blood for a substance called C-reactive protein. The body releases C-reactive protein when blood vessels leading to the heart are damaged by atherosclerosis. The level of C-reactive protein in the blood helps doctors predict the patient’s risk of heart attack. Depending on the results, they may advise people to quit smoking or to follow a special diet to control high blood pressure, cholesterol level, or weight.
Symptoms and diagnosis.
Most coronary atherosclerosis develops over many years. Doctors have found the beginnings of plaques in arteries of young soldiers killed in battle. But symptoms seldom occur until age 50 or later, when arteries have narrowed more than 50 percent. In some cases, a heart attack or sudden death occurs in a person who had no previous symptoms. But many people experience an early symptom called angina pectoris, or simply angina. Angina is pain in the chest that happens during exercise or some other activity that makes the heart work harder than usual. Angina occurs because diseased coronary arteries supply the heart with too little oxygen. This lack of oxygen makes the heart muscle hurt during hard work. After the exercise or other activity stops, the pain usually disappears. However, untreated angina may worsen and cause pain even when patients are resting.
Physicians diagnose coronary artery disease by first asking patients about their general physical condition and any past illnesses. The physicians note any risk factors, such as a history of angina or heart attack in the patients or members of their families. Physical examination may reveal additional risk factors, such as high blood pressure or a high cholesterol level.
One of the most useful tools for diagnosing CAD is an instrument called an electrocardiograph. This instrument produces a record called an electrocardiogram (ECG), which displays the electrical activity of the heart muscle. This record is printed on moving paper that shows the electrical activity as a series of wavy lines.
Major waves represent contraction of the ventricles. Minor waves represent relaxation of the ventricles and contraction and relaxation of the atria. Most ECG’s are recorded with the patient lying down. However, many physicians take a patient’s ECG during exercise. Such a stress ECG shows whether a patient’s heart—even if the patient has no chest pain—receives enough oxygen during vigorous exercise. See Electrocardiograph.
Doctors also use a method called radionuclide imaging to detect CAD. In this procedure, a doctor injects a radioactive element into a patient’s bloodstream. The doctor can view the element on a screen as it spreads into the heart muscle. Areas that do not receive blood appear blank on the image. Doctors generally use radionuclide imaging with a stress ECG.
A type of computed tomography (CT), commonly called a heart scan, is sometimes used to detect calcium deposits in coronary arteries. Such calcium deposits may indicate a risk for heart disease in some people.
If these diagnostic techniques leave doubt about the presence of CAD, physicians may perform cardiac catheterization followed by coronary angiography. In these tests, doctors insert a long, flexible tube called a catheter through a large blood vessel, usually an artery in the area where the thigh and abdomen meet. They push the catheter up to the beginning of the coronary arteries, then inject a special dye. The dye clearly shows the condition of the arteries as it travels through them. An image of the arteries can be recorded on an X-ray film called an angiogram. Doctors perform angiography only when diagnosis is difficult, because it carries a small risk of injury or death. See Angiography.
Treatment.
Coronary artery disease cannot be cured. But doctors can treat many patients with drugs or surgery to limit the effects of CAD on their lives. Doctors evaluate each patient with CAD to determine which treatment would provide the greatest benefit. In many cases, physicians also advise patients to exercise, reduce their intake of fat and calories, and take other steps to help slow development of CAD.
Several drugs can relieve angina. A drug called nitroglycerin can stop angina pain within two minutes. When nitroglycerin tablets are dissolved under the tongue, they expand coronary arteries and enable more blood to flow past fatty deposits. Drugs called beta-blockers and calcium channel blockers may also prevent angina. Beta-blockers slow the action of the heart and reduce its contracting force. The heart’s demand for oxygen then decreases, making it easier for the heart to pump. Calcium channel blockers have a similar effect on the heart and also relax the coronary arteries. These two drugs also reduce high blood pressure.
A group of drugs called statins—for example, lovastatin, sold under the trade name Mevacor—helps lower blood cholesterol levels. Many doctors advise CAD patients to take one aspirin tablet a day. Aspirin thins blood and can help prevent blood clots in coronary arteries.
If drugs fail to control coronary artery disease, doctors consider surgical methods to correct the problem. In one procedure, called coronary angioplasty or simply angioplasty, doctors insert a catheter into the narrowed area of an artery. The catheter has a small deflated balloon attached to the end. Doctors then inflate the balloon, which compresses the plaque against the arterial wall and enlarges the artery. Angioplasty works at first in about 85 percent of patients. But in about a third of these patients, blockage returns within three months. For some patients, various methods may prevent new blockage and prolong the benefits of angioplasty. For example, tiny metal tubes called stents may be placed in the artery to keep it propped open. See Angioplasty.
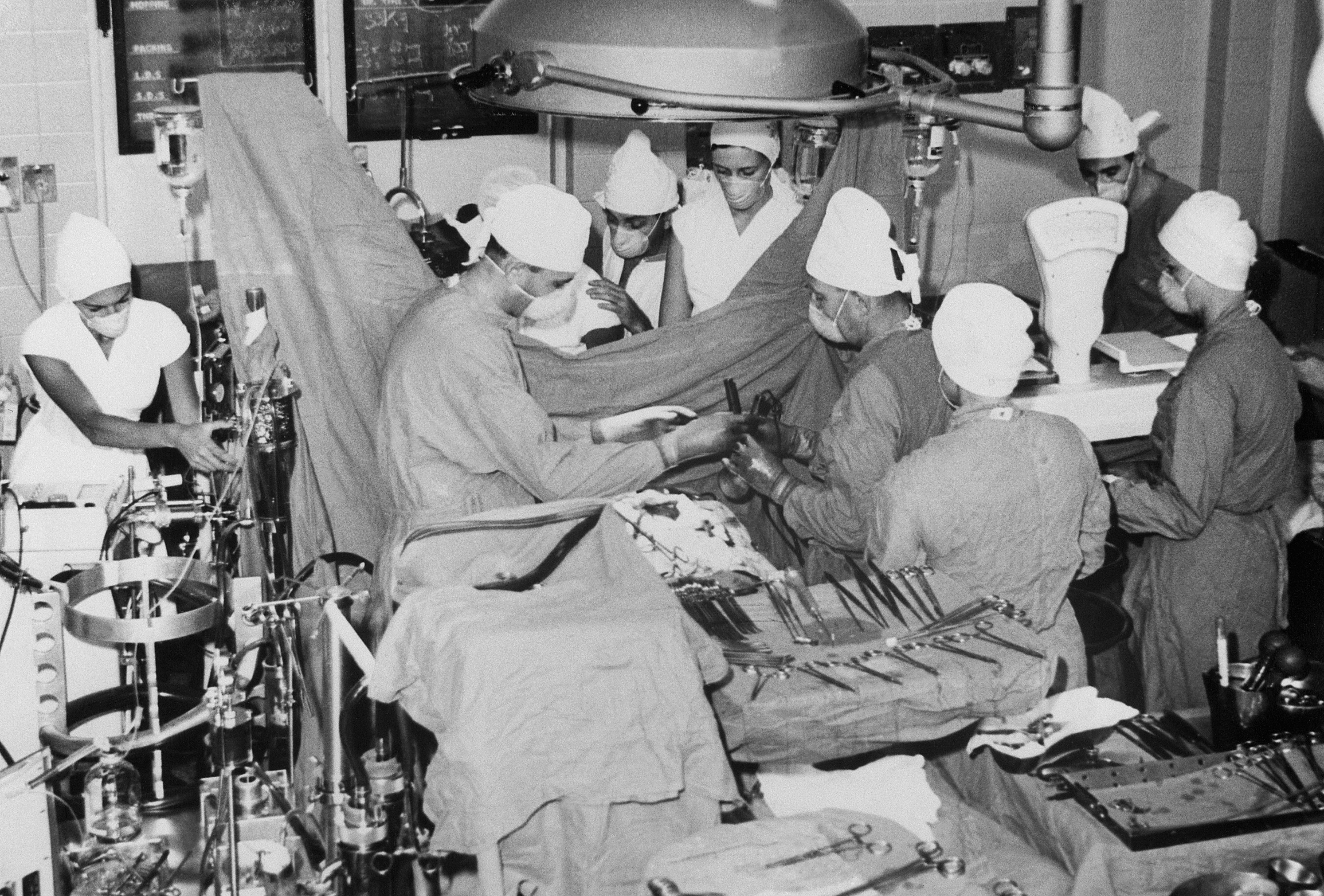
If catheter treatments fail, most cardiologists suggest a more serious procedure called coronary bypass surgery. Bypass surgery uses a replacement blood vessel from the patient’s own body to carry blood around a blockage in one or more coronary arteries. In most such procedures, doctors redirect an artery that branches from the aorta to another part of the chest. They cut the part of the vessel that leads to the chest, then reattach that end to the affected coronary artery, bypassing the blocked section. A coronary bypass can ease symptoms of angina and prolong life for patients with severe CAD. But it does not stop atherosclerosis.
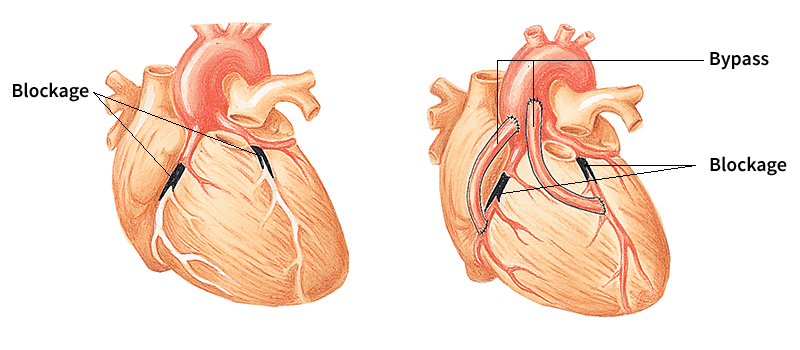
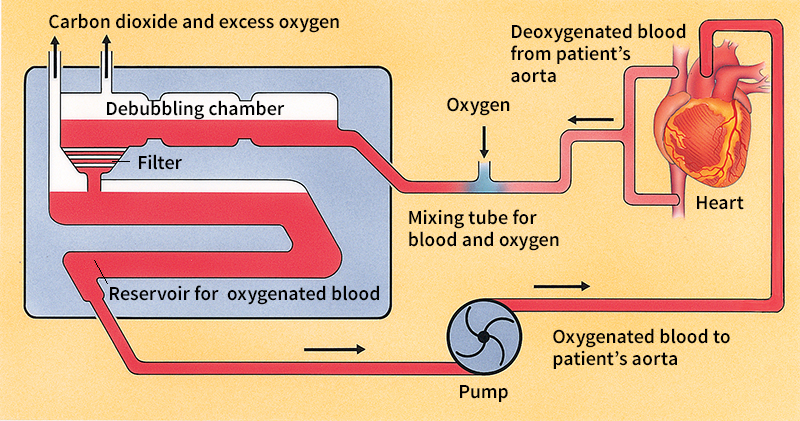
During most bypasses, surgeons stop the heart and use a device called a heart-lung machine to take over the work of those organs. This device uses a system of membranes to exchange carbon dioxide in the blood for oxygen. An electric pump then delivers the oxygenated blood to the body. Surgeons are working to perfect techniques that avoid use of the heart-lung machine and enable them to operate directly on the beating heart.
Heart attack
Almost all heart attacks occur when a blood clot suddenly and completely blocks a coronary artery. This condition is called a coronary thrombosis, or simply a coronary. The part of the heart muscle nourished by the blocked artery becomes damaged by lack of oxygen. Unless blood flow returns within minutes, muscle damage increases. Heart cells begin to die after four to six hours without blood. The damage can affect the heart’s ability to pump and may cause the patient’s death. If the clot can be dissolved within four to six hours, damage to the heart can be reduced.

Symptoms.
Some people have no warning signs at the beginning of a heart attack. But many people experience angina, dizziness, indigestion, or other symptoms. Most heart attacks cause severe pain. Patients describe the pain as a dull, crushing ache in the chest, but discomfort may extend into the neck, jaw, arms, or back. The pain may last from a few minutes to several hours.
Anyone with chest pain who suspects the pain may be due to a heart attack should seek medical help immediately. Some patients may stop breathing, and their hearts may stop beating. A first-aid technique called cardiopulmonary resuscitation (CPR) can maintain breathing and circulation until a patient can be taken to a hospital. But CPR should be performed only by someone trained in the technique. See Cardiopulmonary resuscitation.
Diagnosis and treatment.
Injured heart muscle causes abnormal ECG waves. Soon after a patient reaches the hospital, doctors administer an ECG to determine that symptoms result from a heart attack and not some other disorder. Doctors also use certain blood tests to detect a heart attack. But these tests are not useful until a few hours after an attack.
Doctors may administer a strong painkilling drug, such as morphine, to relieve the pain of a heart attack. They also use drugs to dissolve clots in the blocked artery or may perform emergency angioplasty or bypass surgery.
After doctors stabilize the condition of a heart attack patient, they admit the person to the hospital and monitor him or her for complications in the intensive care unit. Some hospitals have a specialized intensive care unit called a coronary care unit for heart patients. Two major complications are heart failure and arrhythmia. Heart failure occurs if the heart cannot pump enough blood because of extensive damage to the heart muscle. In most cases, heart failure can be successfully treated. In arrhythmia, the heart’s electrical system produces an abnormal pattern of beats. Most arrhythmias can be readily treated, but a type called ventricular fibrillation can cause sudden death. Ventricular fibrillation occurs when electrical signals in the ventricles fire randomly.
More than 20 percent of heart attack patients who do not get medical care die. Some people die before they can reach a doctor, but other patients ignore their symptoms and delay treatment. The death rate among hospitalized patients ranges from 5 to 10 percent. Heart attack patients with ongoing chest pain, arrhythmias, or heart failure have a greater risk of another attack than do patients without these problems.
Recovery.
Many doctors perform stress tests on patients who have had a heart attack to determine their risk of having another attack or dying suddenly. Patients with abnormal stress tests may be advised to consider angioplasty or bypass surgery. People without complications are sent home for recovery and rehabilitation. Rehabilitation seeks to restore good health through a program that includes gradual increase in exercise and proper diet. The program may also include drugs to control such conditions as high blood pressure and high cholesterol. Most patients can do light work in 30 days. Complete recovery from an attack that leaves thick scars on the heart may take up to three months.
Birth defects
Heart disorders present at birth are called congenital heart disease. About 8 of every 1,000 babies have such abnormalities, which may be minor or so severe they are fatal. Defects occur as a baby’s heart forms during its first few weeks of development in its mother’s body. Doctors do not know what causes many congenital defects, but they think that some are due to genetic flaws. For example, the risk of having a congenital disorder increases for babies whose mothers have such defects. Other cases may occur as a result of certain illnesses in the mother or her use of medications. The first sign of a congenital defect may be an unusual sound called a heart murmur (see Heart murmur). Most such defects involve either abnormal openings in the heart or narrowed sections that block the flow of blood. Many of these disorders can be corrected surgically.
Abnormal openings in the heart.
Some of the most severe congenital heart disorders are septal defects—that is, holes in the septum. A hole between the atria is an atrial septal defect (ASD), and one between the ventricles is a ventricular septal defect (VSD). Such holes allow oxygenated blood from the left side of the heart to enter the right side. When oxygenated blood recirculates to the lungs, it can cause congestion. Surgeons can correct both defects. VSD’s are more serious than ASD’s because of the extremely high pressure in the left ventricle. Some ASD’s may not be detected until later in life, when blood pressure increases. If a large VSD is not corrected before a child is 2 years old, the lungs may be damaged, causing disability and premature death.
Another abnormal opening results if a blood vessel that enables the blood of unborn babies to bypass their lungs fails to close at birth. This vessel is called the ductus arteriosus or simply ductus. The ductus exists because an unborn baby’s blood does not circulate through its lungs—the baby gets all its food and oxygen from its mother’s body. The ductus carries blood directly from the pulmonary artery to the aorta. The ductus usually closes at birth as the baby’s lungs begin to function.
In a condition called patent ductus arteriosus (PDA), the newborn baby’s ductus stays open. As a result, the blood flow reverses and runs from the higher-pressured aorta to the pulmonary artery. As with VSD, oxygenated blood returns to the lungs, causing congestion. Death may result unless the ductus is closed. Doctors administer drugs to close it. If drugs fail, PDA can be corrected with devices attached to catheters or with surgery.
Blockage of the blood flow
is a common congenital heart defect. One cause of blockage is a condition called bicuspid aortic valve. In this disorder, people are born with an aortic valve that has two flaps instead of three. Two flaps partly block the flow of blood, resulting in a heart murmur. The defect usually presents no serious problem until adulthood, when surgery is required.
Another defect is called coarctation of the aorta, a narrowing of the aorta where it descends to the lower body. This narrowing may cause sudden heart failure in infants. In older children, the defect causes high blood pressure in the arms and head but low blood pressure in the legs. Surgeons usually correct the defect in late childhood, when the aorta is near full size.
An especially complicated congenital heart defect is tetralogy of Fallot, named after Etienne-Louis Fallot, the French doctor who first described the condition. The defect is actually a combination of four disorders—that is, a tetralogy. The two most serious of these disorders are a VSD and a narrowing of the pulmonic valve. The narrowed valve reduces blood flow to the lungs, increasing pressure in the right ventricle. Blood from the right ventricle passes through the VSD to the left ventricle and returns to the body. Because that blood has not flowed through the lungs and acquired the red color of oxygenated blood, it makes the skin appear bluish. As a result, babies who have this defect are called blue babies. Some blue babies can be treated with drugs, but most need surgery to correct the condition. See Blue baby.
Other heart disorders
Valve disease.
Most valve disorders result from congenital heart defects. Valve disease can also develop if the flaps of the heart valves become scarred or deformed. There are two main types of valve disorder. A narrowing of the valve opening called stenosis occurs if the flaps harden. Stenosis may reduce the flow of blood through the valve. Regurgitation, also called insufficiency, arises if the flaps close improperly and permit blood to leak back into the chamber from which it came. Valve disorders may not appear until adulthood, after years of wear on the deformed valve begin to affect its function.
One common valve disorder is mitral valve prolapse. In this condition, the flaps of the mitral valve are slightly larger than normal and fail to close properly. Many people with mitral valve prolapse have no serious symptoms, but significant regurgitation occurs in some cases.
An illness called rheumatic fever once caused many cases of valve damage, especially to the mitral valve. Rheumatic fever is a serious reaction that can follow infection with certain streptococcus bacteria, including some that cause strep throat. Rheumatic fever has become uncommon in developed countries because most strep infections are now promptly diagnosed and treated with antibiotics. See Rheumatic fever.
Symptoms of valve disease include shortness of breath during exercise, tiredness, continual cough, and occasional chest pains. Doctors can make a preliminary diagnosis of valve disorders by detecting heart murmurs, sounds which result from disturbed blood flow. Regurgitation or the slowed passage of blood through a narrowed valve cause the disturbed flow.
Doctors use several methods to confirm the diagnosis and to determine the seriousness of valve disease. A technique called echocardiography sends ultrasound waves through the chest. The sound waves bounce off the heart, and the returning echoes are transformed into a video image of the heart’s valves and other structures. Doctors also use this technique to detect disturbed blood flow, coronary artery disease, and other conditions. If echocardiography still leaves doubt about the existence of valve disease, doctors perform cardiac catheterization along with angiography.
Doctors closely monitor patients with diseased valves for any changes in symptoms. If the disorder worsens, regurgitation and stenosis may cause congestive heart failure, a condition in which the heart cannot pump enough blood. Doctors treat congestive heart failure several ways. They may ask patients to rest frequently, lose weight, or follow other advice to reduce the heart’s workload. In many cases, doctors prescribe drugs called angiotensin converting enzyme inhibitors or certain other drugs to improve the heart’s pumping ability.
If nonsurgical methods of treatment fail, doctors operate to repair or replace the valve. A diseased aortic valve is especially likely to need replacement. Surgeons use several types of artificial valves. One type, the bileaflet valve, consists of two semicircular carbon disks that open by means of a pivot mechanism. Another replacement valve comes from a pig’s heart. It works much like a human heart valve. In some cases, the semilunar valves and portions of the great vessels can be replaced with transplants from donors. See Transplant.
Abnormal heart rhythms,
called arrhythmias, can range from harmless to deadly. An ECG can detect most abnormal rhythms. An arrhythmia slower than 60 beats per minute is called bradycardia. One faster than 100 beats per minute is called tachycardia.
Bradycardia may result from disease or drugs that slow the heart’s natural pacemaker, which sets the heart rate by means of rhythmic electrical signals. Blockage of the electrical signal along the heart’s conducting pathways produces a bradycardia called heart block. If heart block cannot be treated in any other way, doctors insert an electronic artificial pacemaker near the heart. This battery-operated device delivers a steady electrical signal to the heart. A pacemaker can vary its rate, depending on the person’s activity level.
A tachycardia occurs if disease causes the atria or ventricles to send electrical signals too rapidly. Atrial tachycardias are relatively easy to treat. But ventricular tachycardias may lead to a condition called fibrillation in which disorganized contractions cause sudden death. Several drugs can stop tachycardias. If drugs fail to work on the ventricles, doctors can insert an electrical device similar to a pacemaker to overcome fibrillation. The device, called a defibrillator, senses when a ventricular tachycardia occurs and delivers a small shock to stop it.
Inflammatory heart disease
results from conditions that cause pain and swelling in heart tissues in response to certain activities of the immune system. Pericarditis is inflammation of the pericardium, the membrane that surrounds the heart. It can result from infectious diseases, arthritis, kidney failure, or other disorders. Pericarditis may cause fluid to collect under the pericardium. If too much fluid accumulates, the pericardium compresses the heart so that it cannot pump enough blood to the body. The condition may cause death unless doctors drain the fluid with a needle pushed through the chest and into the pericardium. Repeated inflammation can scar the pericardium and squeeze the heart. Surgeons remove such scar tissue.
The endocardium, the membrane that lines the heart’s chambers and makes up its valves, becomes inflamed in a disease called bacterial endocarditis. This condition arises when bacteria that normally grow harmlessly in other parts of the body enter the bloodstream and infect the heart. For example, bacteria from the mouth may enter the blood during dental surgery. In most people, normal body defenses destroy such bacteria. But in patients with valvular disease, bacteria may collect on the abnormal valve and grow. Bacterial endocarditis is fatal unless it is treated with antibiotics. To prevent endocarditis, doctors give antibiotics before and after surgery to patients who have a high risk of infection.
Inflammation of the myocardium, the muscle tissue that forms the heart’s walls, is called myocarditis. If the inflammation damages the muscle cells beyond repair, a patient with myocarditis may require a heart transplant.
Cardiomyopathy
refers to any of various diseases that affect the heart muscle itself. There are two general forms of this disorder. In hypertrophic cardiomyopathy, heart muscle tissue grows excessively thick. In congestive cardiomyopathy, the heart muscle becomes weakened and causes heart failure.
Most cases of hypertrophic cardiomyopathy involve thickening of the septum between the heart’s two lower chambers. The thickened septum blocks blood flowing from the left ventricle, causing lung congestion. The condition can be treated with drugs that relax the heart and reduce the tendency of the extra tissue to block the flow of blood. But if the disease becomes severe, surgeons must cut out the abnormal muscle.
Congestive cardiomyopathy occurs if heart muscle weakness causes the left ventricle to enlarge, resulting in inadequate pumping. In most cases, doctors do not know the cause of congestive cardiomyopathy. They have no specific treatment for the condition but may prescribe certain drugs and restrict a patient’s activities to slow the progress of the disease. Some patients may need a heart transplant.
Heart failure
is a disorder in which the heart pumps inefficiently. It does not mean that the heart stops beating. The organ’s contractions may become weakened, or its chambers may enlarge or become less able to fill with blood. Any disease that hampers the heart’s ability to deliver blood to the body may cause the condition. Most cases result from coronary artery disease, cardiomyopathy, or valve disease. The inadequate blood flow produces exhaustion. In addition, the poor flow makes the blood back up in the lungs. This congestion causes shortness of breath.
The body reacts automatically to try to overcome heart failure, but many of its efforts only worsen the condition. For example, the body tries to maintain blood flow to the brain and other vital organs by narrowing arteries to the arms, legs, and other less essential parts. But contraction of these vessels makes it even harder for the heart to pump.
Drugs are one of the main treatments for heart failure. The oldest such medicines are digitalis drugs, which doctors have prescribed for certain heart conditions for more than 200 years. Digitalis strengthens the heart’s contractions, thus increasing blood flow. Much newer drugs called vasodilators block the body’s natural but undesirable response that tightens certain arteries when heart failure occurs. Some vasodilators relax the smooth muscle in the blood vessel walls. Others block the chemical reactions that make these smooth muscles contract. Drugs that block these chemical reactions include angiotensin converting enzyme inhibitors, which are the main treatment for failure of the left ventricle.
If drugs cannot control heart failure, doctors may operate to correct any problems that led to the disorder. But surgery presents a high risk for dangerously ill patients who do not respond to drugs. Such patients may be connected to temporary cardiac assist devices, which are small pumps attached to the veins and arteries. These devices help the heart do its work and enable surgeons to perform necessary repairs.
If there is no problem that can be corrected surgically, doctors may perform a heart transplant. In this procedure, surgeons replace the patient’s failing heart with a donated heart from the body of someone who has died. But the patient’s body may reject the new heart because the body’s immune system attacks most foreign tissues. Doctors try to prevent rejection with powerful drugs, but these drugs may have serious side effects.
The survival rate for heart transplant patients in the first year after surgery is about 80 percent. Survival requires extensive care and close medical supervision. Many patients who need a transplant die waiting for a suitable heart because there is a shortage of donors. See Transplant.
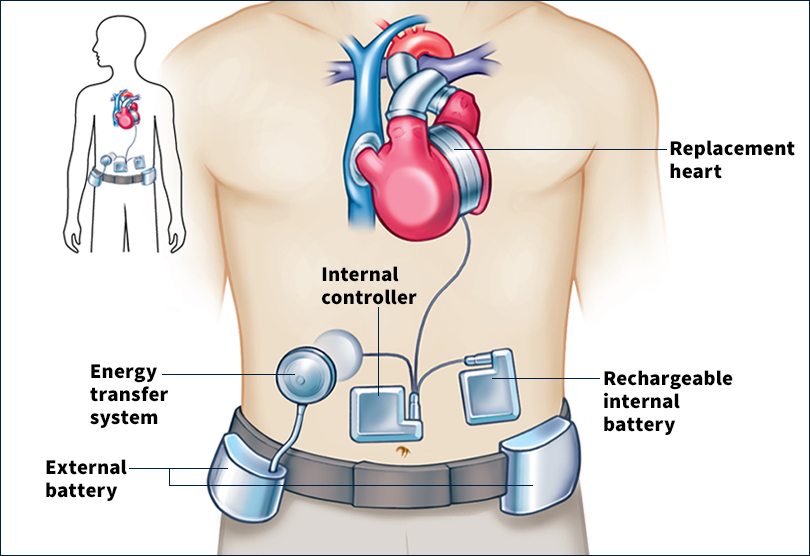
During the 1980’s, surgeons experimented with implanting artificial mechanical hearts in people. However, the devices proved unsuccessful because they tended to form blood clots. See Artificial heart.
History of heart research
Early beliefs about the heart.
Many people in ancient times believed that the heart had special importance. For example, the Chinese thought that each emotion originated in a certain organ and that happiness dwelt in the heart. Chinese physicians diagnosed many illnesses and prescribed treatment by taking the pulse at the wrist. The ancient Egyptians considered the heart to be the source of intelligence and emotion.

The ancient Greeks learned from battlefield injuries and animal sacrifices that the heart was a beating organ. In the A.D. 100’s, the Greek physician Galen developed the first medical theories based on scientific experiments. Galen observed the heartbeat and realized that the heart put blood in motion. But he thought that the heart’s right ventricle forced blood into the left ventricle through holes in the septum. Galen also believed that the liver converted food into blood, which then flowed through the body and was used up. See Galen.
Discovery of circulation.
Doctors accepted Galen’s theories—in spite of their many errors—until the 1500’s. In the mid-1500’s, a Flemish-born physician named Andreas Vesalius described veins and arteries. He also showed that no holes in the septum connect the heart’s chambers. Also in the 1500’s, Michael Servetus, a Spanish physician and theologian, reasoned that blood flows between the heart and lungs.
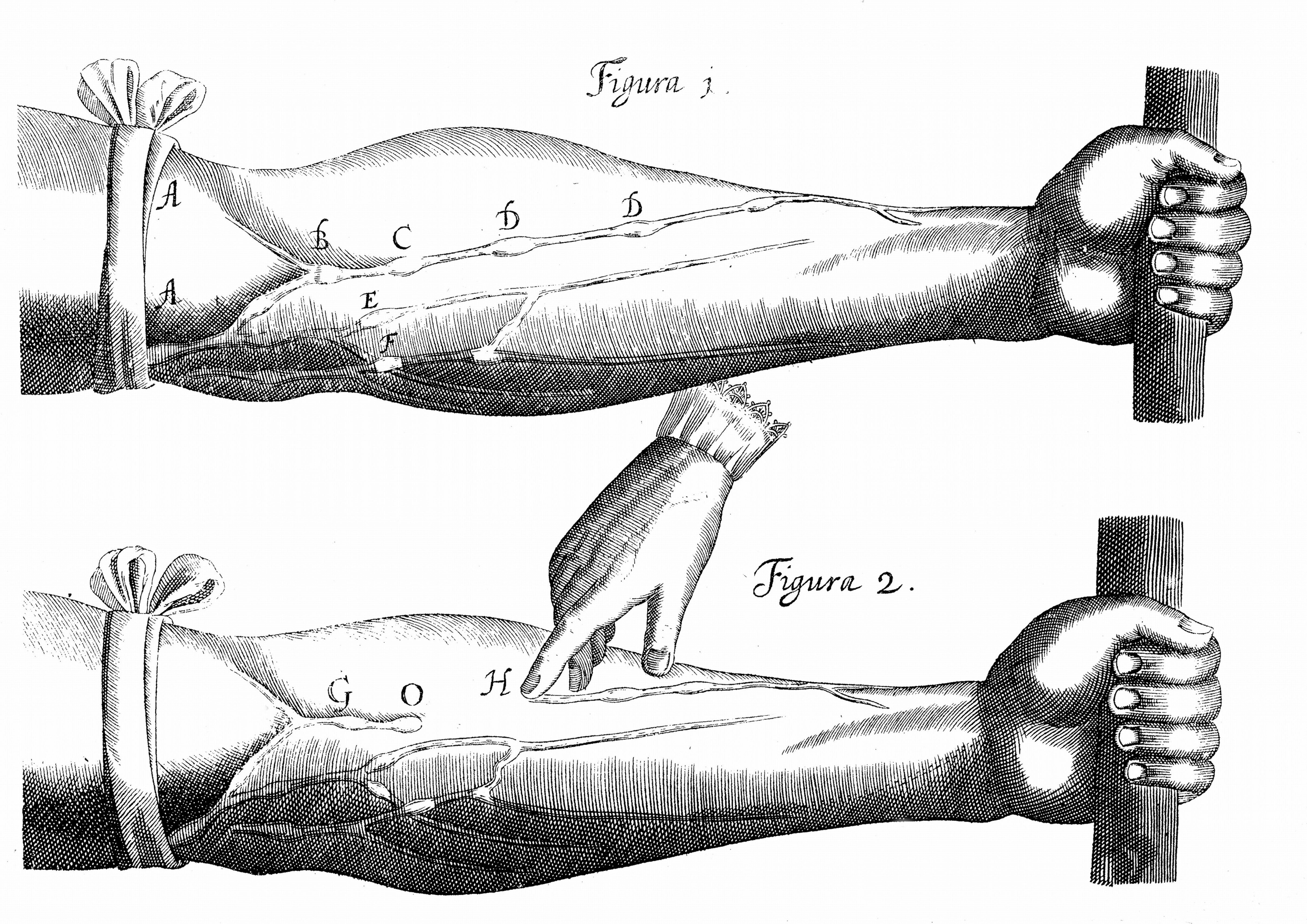
The theory of blood circulation was first published in 1628, by William Harvey, an English physician. His work became the basis of modern research on the heart and blood vessels. Harvey showed that the heart works like a pump. He described how blood flows from the heart to the lungs, back to the heart, out to the body, and back to the heart. Harvey believed that small blood vessels called capillaries connect arteries and veins. The idea of capillaries had been proposed in the 1500’s by an Italian anatomist named Andrea Cesalpino. Marcello Malpighi, an Italian physician, proved their existence in 1661.
In the early 1700’s, Stephen Hales, an English clergyman and scientist, became the first person to measure blood pressure. He placed a glass tube in a horse’s artery after breaking through the animal’s skin. Hales published the result of this experiment in 1733.
Invention of new medical instruments.
During the 1800’s, many inventions expanded doctors’ knowledge of the heart and helped in their diagnosis and treatment of heart problems. In 1816, a French physician named Rene Laënnec invented the stethoscope, which improved doctors’ ability to listen to sounds of the heart and other organs. In 1880, Samuel Siegfried von Basch, a Viennese physician, developed the sphygmomanometer << `sfihg` moh muh NAHM uh tuhr >>, an instrument that could measure blood pressure without breaking the skin. Russian physician Nikolai Korotkoff used a stethoscope in 1905 to take the pulse while measuring blood pressure, thus recording systolic and diastolic blood pressure. Doctors still use this technique.
In 1903, Willem Einthoven, a Dutch physiologist, invented the string galvanometer. This device, which measures electrical currents generated by the activity of the heart, became the basis of the electrocardiograph. By the 1920’s, the electrocardiograph had become the chief diagnostic tool in cardiology.
Development of heart surgery.
In 1912, an American cardiologist named James B. Herrick made the first diagnosis of a heart attack. In 1938, Robert E. Gross, an American surgeon, performed the first successful repair of a congenital heart defect in a child with patent ductus arteriosus. Helen Brooke Taussig and Alfred Blalock, two American physicians, first performed an operation in 1944 to help correct abnormal circulation in blue babies.
In 1952, American surgeon Charles Hufnagel operated on a beating heart and implanted the first artificial heart valve. Another American surgeon, John H. Gibbon, and his associates developed the heart-lung machine. This important advance enabled doctors to stop the heart while the device pumped and oxygenated the blood. Doctors could then repair defects that could not be corrected with the heart beating. Gibbon and his team first used the machine successfully in 1953.
F. Mason Sones, Jr., an American surgeon, performed the first angiography in 1958 and gained the first view of blockages caused by CAD. The coronary bypass operation was perfected in the late 1960’s by Rene Favaloro, an Argentine physician working in the United States. In 1967, American surgeons Michael DeBakey and Adrian Kantrowitz successfully implanted the first cardiac assist device. This device temporarily helped a diseased or overworked left ventricle.
The first heart transplants and artificial hearts.
A team of South African surgeons headed by Christiaan Barnard performed the first human heart transplant in 1967. The patient lived 18 days, then died of a lung infection. Norman Shumway pioneered heart transplants in the United States. He and his surgical team performed the first U.S. heart transplant on an adult patient in 1968. Shumway refined transplant techniques and performed more transplants than any other surgeon up to that time.

In the late 1960’s and early 1970’s, doctors performed many heart transplants. But most patients died within a year, mainly because the body rejected the new organ. As a result, surgeons almost stopped performing these operations. Then in the 1980’s, doctors began using a drug called cyclosporine to fight rejection. Cyclosporine greatly increased the survival rate among transplant patients. The shortage of donor hearts has become the chief obstacle to successful heart transplants today.
Lack of donor hearts has raised interest in mechanical artificial hearts. In 1982, an American surgical team headed by William DeVries implanted the first permanent artificial heart in a human patient. Robert Jarvik, an American physician, designed the device. The patient, Barney Clark, experienced many complications and died 112 days later. A number of other patients received the Jarvik heart, but none survived for as long as two years. In 1990, the U.S. Food and Drug Administration withdrew approval of the Jarvik device. Another model, similar to the Jarvik, is used as a temporary replacement heart at a few medical centers in the United States. In 2001, doctors implanted a new type of artificial heart in a seriously ill patient. Unlike other models, it was completely self-contained and thus did not require any tubes or wires to be run through the patient’s skin.
In the 1990’s, efforts to help patients awaiting transplants focused on a partial artificial heart called a left-ventricular assist device (LVAD). An LVAD takes over the work of the heart’s main pumping chamber—the left ventricle—while the rest of the heart continues to function. LVAD’s have helped some patients survive until donor hearts are available. Doctors hope that LVAD’s may one day offer a permanent transplant alternative.
Progress in treatment and prevention
occurred about the same time as the dramatic advances in heart surgery. In the late 1960’s, researchers developed drugs called beta-blockers. These drugs help reduce high blood pressure, prevent angina, and control certain arrhythmias. Calcium channel blockers, which have similar benefits, appeared in the 1970’s.
In 1977, a Swiss physician named Andreas R. Gruentzig performed the first angioplasty, a nonsurgical procedure to open a blocked artery. Researchers also developed stents and other techniques to use with angioplasty to prolong its effectiveness.
The first implantable defibrillator became available in 1985. This device senses a serious, rapid arrhythmia of the ventricles and sends a small electrical shock to restore a normal heartbeat. Another method, called radiofrequency catheter ablation, has also been developed to treat some rapid arrhythmias. In this procedure, doctors insert a catheter with an electrode tip into the heart. A small current delivered through the electrode destroys the tiny area of heart muscle causing the rapid rhythm.
Much knowledge about preventing heart disease comes from extensive research. For example, the Framingham Heart Study has examined the functioning of the heart in more than 10,000 men and women. This study began in 1948 in Framingham, Massachusetts. Its results have revealed the strong connection linking high blood pressure, high cholesterol, cigarette smoking, and other risk factors with CAD. The main shortcoming of this study is that its participants are almost all white people of similar income levels. Researchers now try to design studies to include people from a variety of ethnic groups and levels of wealth. Such diversity helps ensure that a study’s conclusions apply to everyone. See Framingham Heart Study.
Many preventive efforts focus on using known methods and finding new ones to reduce or eliminate controllable risk factors. For example, many people have their blood pressure and cholesterol level checked regularly. Patients with mild high blood pressure may reduce it by limiting their intake of salt and calories. Others may lower their cholesterol by watching the amount of cholesterol, saturated fat, and calories in their diet. In addition, growing numbers of people exercise regularly, which helps lower cholesterol and blood pressure by keeping body weight down. Drugs to reduce blood pressure and cholesterol help many patients who cannot control these factors with behavior changes.
Hearts of animals
Animals without a backbone.
Many animals without backbones lack a definite heart. Instead, large blood vessels contract rhythmically, pushing blood through their bodies. These blood vessels have valves, which make blood flow in only one direction. Earthworms are one example of animals with this type of circulation.
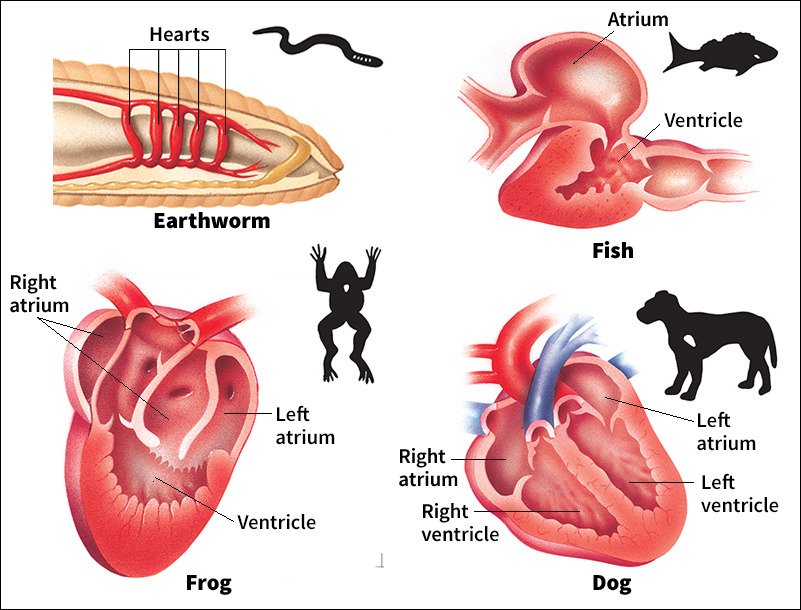
Insects and such animals as spiders, lobsters, and crabs have a one-chambered, tubular heart into which blood flows through holes. The heart then contracts, sealing the holes and pumping blood forward into the arteries. Mollusks, such as clams and snails, have a more complicated heart with one or more atria and a ventricle. The atria, which have thin walls, receive blood from the digestive system and from the mollusk’s muscular burrowing organ called the foot. The atria then pump blood into the thicker-walled ventricle, which sends the blood to the arteries.
Fish
have a two-chambered heart with an atrium and a ventricle. Blood from the body drains into an area called the sinus venosus, flows into the atrium, and then enters the ventricle. From the ventricle, blood passes to an area called the conus arteriosus and then to the aorta. Blood is then pumped from the aorta to the arteries. Blood flows through the arteries to the gills, where it releases carbon dioxide and takes up oxygen.
Amphibians and reptiles.
Adult amphibians and most reptiles have a three-chambered heart with two atria and one ventricle. One atrium receives blood from the body, and the other receives it from the lungs. Both atria pump into the same ventricle. When it contracts, a ridge within the ventricle directs most of the oxygen-rich arterial blood to the body and most of the oxygen-poor venous blood to the lungs.
Birds and mammals
have a four-chambered heart, the most highly developed type. The human heart is a typical mammalian organ. Such a heart powers two types of circulation. Pulmonic circulation sends oxygen-poor blood to the lungs, and systemic circulation delivers oxygenated blood to the body. Such a circulatory system is exceptionally efficient and can pump blood at high pressure.
A bird’s or mammal’s heart rate depends mostly on the animal’s size. The smaller an animal is, the faster its heart beats. For example, a hummingbird has a heart rate of about 1,000 beats per minute. An elephant’s heart beats about 25 times a minute.
