Obesity, << oh BEE suh tee, >> is the condition of having an excessive amount of body fat. Obesity increases a person’s risk for many conditions and diseases, including diabetes, heart disease, hypertension (high blood pressure), arthritis, and cancer. Physicians typically use a simple, inexpensively obtained measurement called the body mass index (BMI) to determine if a person is overweight or obese. The body mass index represents the proportion between a person’s weight and height.
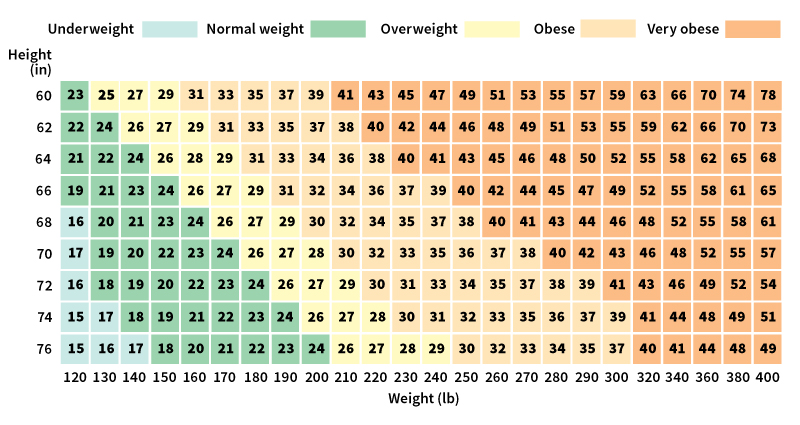
You can calculate your BMI by dividing your weight in kilograms by the square of your height in meters. For example, a woman weighing 130 pounds (59 kilograms) who is 5 feet 4 inches (1.6 meters) tall has a BMI of about 23—that is, 59 divided by 2.56 (or 1.62). Another way to calculate your BMI is to multiply your weight in pounds by 703 and then divide that figure by the square of your height in inches. In adults, a BMI of 25 to 29.9 indicates that the individual is overweight and a BMI of 30 and above indicates obesity.
In children, the normal range of BMI varies with age and differs between boys and girls. Physicians do not have a standard definition of obesity for children, often using the terms obese and overweight interchangeably. To determine if a child is overweight, physicians use growth charts that compare BMI with age, called BMI-for-age charts. They use separate BMI-for-age charts for boys and girls. A physician locates a child’s BMI on the appropriate chart, then compares it to statistical rankings called percentiles, which are shown as curved lines. Physicians consider a child overweight if the child’s BMI-for-age is equal to or greater than the 95th percentile. A ranking in the 95th percentile means that the child’s BMI is higher than that of 95 percent of other boys or girls at the same age. A BMI score in the 85th to 95th percentile indicates a risk of becoming overweight.
Rates of obesity vary widely throughout the world. People in industrialized countries tend to be heavier than people who live in less developed countries. The rate of obesity is rising in many countries. In 2013, the American Medical Association declared obesity to be a disease that requires medical treatment. In the early 2020’s, the Centers for Disease Control and Prevention (CDC) estimated that about two-fifths of adults and about one-fifth of children and adolescents in the United States were obese.
Causes of obesity
Obesity results from an energy imbalance in which a person consumes more calories in food and drink than he or she burns (uses as energy) over time. Genetic and environmental factors influence how much a person eats and how many calories the person burns. In some cases, obesity may result from specific diseases, such as Prader-Willi syndrome, a condition that includes an uncontrollable urge to eat. Hormone imbalances or medications may also cause obesity in some people. However, these causes account for relatively few cases of obesity and are not related to the increase in obesity occurring in the United States and many other countries. Medical experts link the overall rise in obesity to changing lifestyles.
A person’s genetic makeup helps determine the person’s body size, build, and metabolism, the ability of the body to convert food into energy and living tissue. However, personal choices about food and beverage consumption and physical activity can affect a person’s weight. Medical experts know that some behaviors and habits are associated with higher rates of overweight and obesity. These include eating fatty foods, not getting enough fruits and vegetables, skipping breakfast, frequently eating at fast-food restaurants, eating meals with large portion sizes, and maintaining a sedentary (inactive) lifestyle.
Physical inactivity has become an important cause of obesity. Much of this inactivity results from a modern lifestyle. Many people in industrialized countries work sedentary jobs, which involve sitting or standing still for long periods. People in these countries also tend to engage in social and leisure activities that burn few calories. Such activities include watching television, playing video games, using computers, and traveling by automobile instead of walking or bicycling.
Individual decisions concerning diet and exercise generally determine whether a person will become obese or not. However, societal and environmental factors can significantly influence a person’s decisions and thus can contribute to obesity. In the United States and other developed areas, widespread fast-food restaurants and convenience stores typically offer high-calorie meals and snacks. Food portions of meals served at restaurants often exceed the nutritional amounts recommended for maintaining a healthy weight. Commercial advertisements for foods typically focus on convenient foods that are high in fat, sugar, and calories, influencing eating habits. Suburban communities in the United States often lack sidewalks, making trips by car more convenient and safer than walking or riding a bike. In addition, many inner-city areas lack parks, playgrounds, and other facilities for physical activity and exercise.
Consequences of obesity
Obesity impairs (weakens) the function of many organ systems in the body, such as the circulatory system. The risk of serious medical conditions increases with higher BMI values. Obesity-related health problems include Type 2 diabetes, heart disease, hypertension, high blood cholesterol, back and joint problems, sleep apnea (a condition in which breathing passages are repeatedly blocked during sleep), and certain cancers. In addition, obesity reduces quality of life, complicates recovery from surgery, and contributes to premature death from other causes.
Obesity and obesity-related health problems increase health care costs for individuals and communities. Medical costs associated with obesity include direct and indirect costs. Direct medical costs result from the diagnosis and treatment of obesity and related complications. Indirect costs include the value of income lost because of decreased productivity, restricted activity, and more frequent absences, all of which are associated with obesity. Indirect costs also include the value of future income lost by premature death. Medical experts have suggested that the health care costs related to obesity in the United States are comparable to those associated with smoking.
Social researchers have found that obese people often experience higher than normal rates of discrimination and social isolation. For children, the emotional and social consequences of obesity can include low self-esteem, unfavorable body image, depression, exposure to teasing and discrimination, and social isolation.
Prevention of obesity
Scientists are discovering that tastes, eating habits, and attitudes about diet are established at a young age and often persist throughout a person’s lifetime. In addition, they have found that children who are overweight have a much higher risk of being overweight as adults. Many scientists have therefore concluded that the most effective way to prevent obesity is to prevent unhealthy weight gain beginning in childhood.
Successful prevention programs involve promoting a balanced, nutritious diet and encouraging physical activity for all children, not just those perceived to be overweight. Health experts also emphasize the importance of helping children develop healthy attitudes toward food. They advise encouraging children to learn to recognize internal signals that indicate satiety (fullness) during meals. Parents and caregivers can help by setting a healthy example in their food choices and other eating behavior.
To assist in the development of a healthy lifestyle, the United States Department of Agriculture (USDA) issued a new food guide system in 2011 called MyPlate. The guide outlines dietary recommendations for each food group that can help prevent obesity. The program encourages people to eat more fruits, vegetables, whole grains, lean meats, and fat-free or low-fat milk and milk products. It also emphasizes that a healthy diet should be low in saturated fats, trans fats, cholesterol, salt, and added sugars.
The Dietary Guidelines for Americans, published by the United States Department of Health and Human Services (HHS) and the USDA, recommends that children and teenagers engage in at least 60 minutes of exercise or other physical activity each day. They also suggest that children be as active as possible, Adults should aim for at least 30 minutes of activity daily and should take part in moderate or vigorous activity, such as running or bicycling, three or more times a week.
Public health experts point out that communities can make changes to promote healthy lifestyles and help prevent obesity. For example, communities can encourage people to increase their physical activity by constructing parks, playgrounds, and bike paths. Schools can improve the availability of nutritious foods and beverages, promote nutrition education classes, and offer quality physical education.
Treatment of obesity
Treatments for obesity involve first losing the excess weight. Guidelines published by the United States National Institutes of Health (NIH) recommend weight loss for overweight individuals who have two or more risk factors associated with weight. These risk factors include hypertension, diabetes, and arthritis. Other health care organizations recommend weight loss for all overweight individuals. Specific weight loss goals and methods differ for each individual. For obese adults, treatment should begin with a thorough clinical assessment by a physician. The physician can help develop a behavior modification plan tailored to the individual to promote weight loss. In some cases, drugs and surgery can help in the treatment of obesity. However, medical experts recommend discussing these methods with a physician to explore the risks and advantages.
An important challenge in treating obesity is to prevent excessive weight gain from occurring again in the future. Obesity is a chronic condition. Successful treatment often requires long-term, structured therapy. Support from physicians, caregivers, family, and friends and the appropriate use of medical treatments can increase a person’s chances for lasting success in maintaining a healthy weight.
Changes in behavior.
Medical experts often advise a person who aims to maintain or lose weight to review personal habits and behaviors to determine what improvements can be made. Physicians recommend that anyone beginning a weight-loss program start slowly and set reasonable goals. Initial changes can be as simple as switching from whole milk to low-fat milk or increasing the distance walked each day. A healthy, effective program aims for slow weight loss through a reduction in dietary fat and an increase in physical activity. Researchers have found that such a program can help ensure successful weight loss and long-term weight maintenance.
Surgery.
Some severely obese people require a surgical operation to reduce the size of their stomach or the length of their small intestine. This surgery, called bariatric surgery, has become increasingly common for obese people who cannot lose weight by traditional means or for people who suffer from serious health problems related to obesity. The operation promotes weight loss by restricting food intake or by interrupting the digestive process so that the body cannot absorb many of the calories from food.
Several different types of bariatric surgery exist. Each type of surgery involves some risks and requires patients to make lifelong changes to their diet and lifestyle. A patient should only undergo bariatric surgery after consulting with a physician and carefully evaluating the long-term risks and benefits of the operation.
Treatment for children.
Unless serious health concerns are involved, physicians typically recommend weight maintenance for overweight children rather than weight loss. Medical experts worry that restricting calories to promote weight loss might result in a child consuming inadequate nutrients to sustain healthy growth. Parents and children can work together to identify possible contributors to weight gain, then develop simple weight-maintenance goals. By keeping a steady weight, a child can often outgrow being overweight.
Bariatric surgery is sometimes considered as a treatment option for adolescents who are severely overweight. However, physicians have many concerns about the long-term effects of the surgery on adolescents, who are still developing physically and mentally. Physicians recommend that bariatric surgery be considered only when adolescents are severely obese (a BMI of greater than or equal to 40), have reached their adult height, and have serious weight-related health problems. In addition, they advise that adolescent patients and their parents be evaluated to ensure they are emotionally prepared for the surgery and the lifestyle changes that it requires.
Effects of weight loss.
Weight loss in obese people improves or eliminates obesity-related medical conditions and may also improve quality of life. Many of the results relate directly to the amount of weight lost. Obese people therefore do not have to become lean to benefit from weight loss. Beneficial health effects result from modest weight losses and increase with greater weight loss. Loss of as little as 10 percent of total body weight can produce significant health benefits in an obese person, even if the person remains obese.
See also Bariatric surgery ; Binge eating ; Body image ; Fatty liver disease ; Nutrition (Nutrition guidelines) ; Weight control .
