Sickle cell anemia << uh NEE mee uh >>, also called sickle cell disease, is a hereditary blood disease. In the United States, it occurs chiefly among African Americans. Worldwide, it also affects other groups, including people of Central African, Mediterranean, Middle Eastern, and Indian ancestry. The disease causes moderate to severe anemia, as well as periodic attacks of severe pain and fever called crises. It also disrupts blood flow, which can cause strokes, organ damage, and sudden death.
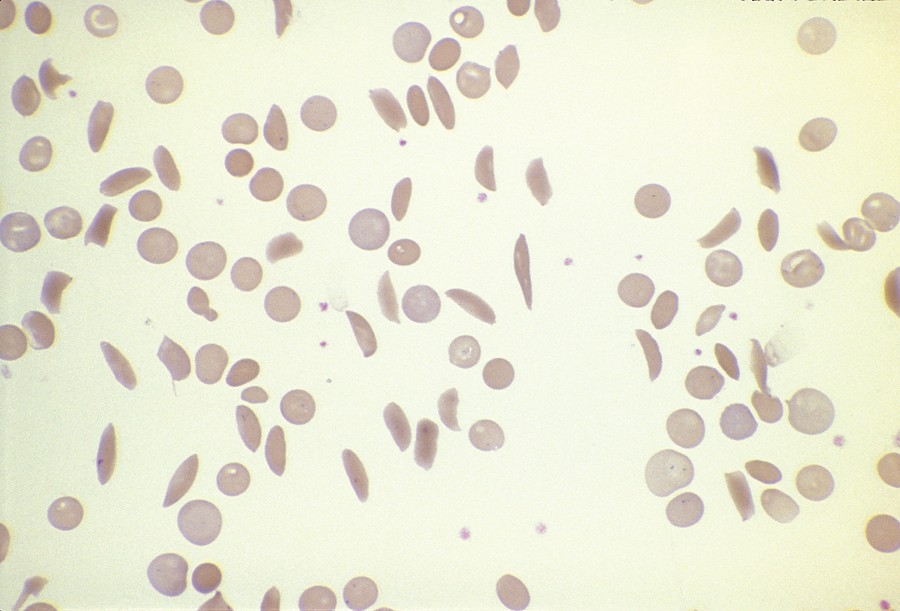
Sickle cell patients have an abnormal type of hemoglobin, the oxygen-carrying protein that gives red blood cells their color. The abnormal protein, called sickle hemoglobin, or hemoglobin S, forms crystals in red blood cells when the cells release oxygen as they flow through tissues in the body. The crystallized hemoglobin causes the normally round red blood cells to change into twisted, rigid sickle forms. The sickle cells can get trapped and block the normal flow of blood through tiny blood vessels called capillaries. This disruption of blood flow causes the periodic crises.
Sickle cell anemia occurs when a child inherits the gene for sickle hemoglobin from both parents. About 1 of every 10 African Americans has one copy of the gene. These people have the sickle cell trait but do not have the disease. About 1 of every 600 African Americans is born with two copies of the gene and has the disease.
Early diagnosis of sickle cell anemia, usually at birth, and antibiotics to prevent infections have greatly improved the survival and life span of people with the disease. Several drugs can reduce the frequency of a patient’s crises, lowering the risk of a life-threatening medical emergency. These drugs include hydroxyurea, L-glutamine, and crizanlizumab. Another drug, voxelotor, also increases the amount of normal hemoglobin in the body.
Some young children with sickle cell anemia can be cured by a bone marrow transplant. Such a transplant involves destroying the patient’s blood-forming tissues with drugs and replacing the tissues using bone marrow stem cells from a healthy donor. The stem cells develop into bone marrow that produces red blood cells with normal hemoglobin. But suitable donors are not always available, and this treatment carries some risk of serious illness or death.
In gene therapy treatments for sickle cell anemia, doctors transfer genetic instructions into a patient’s cells. The instructions stop the body from producing sickle-shaped cells and instruct it to produce healthy cells. Medical researchers think one such gene therapy, based on a CRISPR gene-editing system, may cure sickle cell anemia permanently in some patients. But gene therapy is extremely costly, and few hospitals have the resources to treat gene therapy patients.
See also Anemia; Blood; Bone marrow transplant; Genetic testing; Races, Human (Susceptibility to genetic diseases).
